Peeling skin on the hands is a relatively common problem that, in most cases, does not indicate a serious medical problem. However, it is a source of significant discomfort and stress. Understanding the causes of peeling skin is the key to solving that problem, and it is usually relatively easy.
Causes of Peeling Skin on the Hands
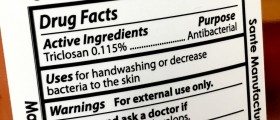
There are many possible causes for this problem, and some of them are really very simple. For example, people who wash their hands too much or use harsh soaps are often affected by this problem. Hygiene is important, but overdoing it can lead to problems like this. Hot water can cause peeling skin, so it is better to use lukewarm water instead.

Certain environmental factors can lead to peeling skin on the hands, such as dry weather, wind, cold, exposure to sun and indoor heating.
- Tinea manuum frequently coexists with tinea pedis, but occasionally, localized forms may affect the hands exclusively. Tinea manuum is distributed worldwide, and, as with other dermatophytoses, other people (anthropophilic), animals (zoophilic), and soil (geophilic) are the most common sources in the United States.
- Tinea manuum is caused by dermatophytes, and the most common agent worldwide is Trichophyton rubrum. However, different etiologic organisms have been reported in various geographical locations.
- An estimated 10% to 25% of the world’s population is infected by a dermatophyte. Of these infections, tinea pedis and manuum are the most common clinical presentations with tinea pedis occurring in up to 70% of adults.
- One study of collected cases of tinea manuum showed that “the two feet, one hand syndrome” is the most frequent (65%) clinical presentation, followed by bilateral tinea pedis with bilateral tinea manuum (19.3%), unilateral tinea manuum (11.8%), and bilateral tinea manuum (3.9%).
- Differences in susceptibility, even when individuals have the same risk factors to fungal infection, provide evidence about the complex interaction between the host, agent, and the environment. Recently, the immune-genetic predispositions for more severe, invasive disease have been described in the literature with specific defects in the innate and adaptative immunity. The cell-mediated immune response is currently accepted as being responsible for the infection control of dermatophytes.
- Several topical and systemic antifungal therapy options and regimens are available. When possible, topical therapy is preferred for tinea manuum due to the risk of drug interactions and side effects of the oral treatments.
- There is no difference in cure rates among allylamines (terbinafine, naftifine), imidazoles (clotrimazole, fluconazole, itraconazole, ketoconazole), or other antifungals, such as butenafine and ciclopirox olamine.
- Making the correct diagnosis and gaining compliance with an appropriate treatment regimen is critical to effecting a mycological cure. Some treatments might require several weeks, so noncompliance is a common reason for treatment failure.
- Relapse or recurrence after therapy remains a concern. Infection transmission from symptom-free carriers, like family and pets, needs to be identified. Adjuvant therapies might be required for adequate control of infection in the treatment-refractory patient and in the carriers, and disinfectant techniques should be employed to control exposure via fomites.
Using chemicals, for example, detergents, fabric softeners and similar products often cause dry skin. Of course, no one wears gloves while hand-washing the clothes, but it helps to thoroughly rinse them after doing so, in order to remove all the residues of the product.
Peeling of the skin on the palms and soles of the feet can sometimes occur after a strep infection, like scarlet fever or after viral infections. In this case, the problem soon goes away on its own.
One serious cause of peeling skin on the hands is vitamin deficiency. The human body reacts in different ways when it does not get enough essential nutrients and peeling skin is one of them. In this case, it helps to increase the intake of all the vitamins and minerals, both through a diet and by using supplements. If the condition does not clear, it is better to see a doctor.
Treatment for Peeling Skin on Hands
Sometimes the skin just needs a little help to shed dead cells. If the skin peels, it means that the dead skin cells are not being removed naturally and it can help to exfoliate the skin to get rid of all of it. This can be done with a cotton towel, some sea salt or even sand and there are of course exfoliating products that work really well. Oatmeal baths are a good natural way to exfoliate, too.
After exfoliating, it is recommended to moisturize. Since dry skin is the major cause of peeling of the skin, it means that moisturizing should be done more often and with better products.
The skin also needs to be nourished from the inside, with a diet that is rich in all the nutrients.
Finally, the skin needs protection from the harsh environment, meaning it is important to wear gloves or mittens in the winter and to apply sunscreen in the summer.
















Your thoughts on this
Loading...