Jugular vein thrombosis may be caused by certain head and neck infections, previous surgery in the area of the vein, central venous catheters, and the nearby presence of certain malignant tumors. It is, however also frequently associated with IV drug abuse. This condition can put patient's life in danger as it carries additional risk of systemic sepsis, pulmonary embolism, chylothorax, papilledema, and other severe complications.
It has been reported that thrombosis of the jugular vein affects patients who have undergone percutaneous insertion of hemodialysis catheters less so compared to those who have undergone surgical insertion of the catheter. This condition may also affect intravenous drug addicts who have exhausted all the available sites on the body and have started to inject drugs right into their jugular vein, in which case it poses an especial diagnostic challenge as this population is resistant to seeking medical care.
Jugular vein thrombosis is common after insertion of central venous catheter. This procedure has to be performed in certain diseases and helps in faster and better administration of some medications.
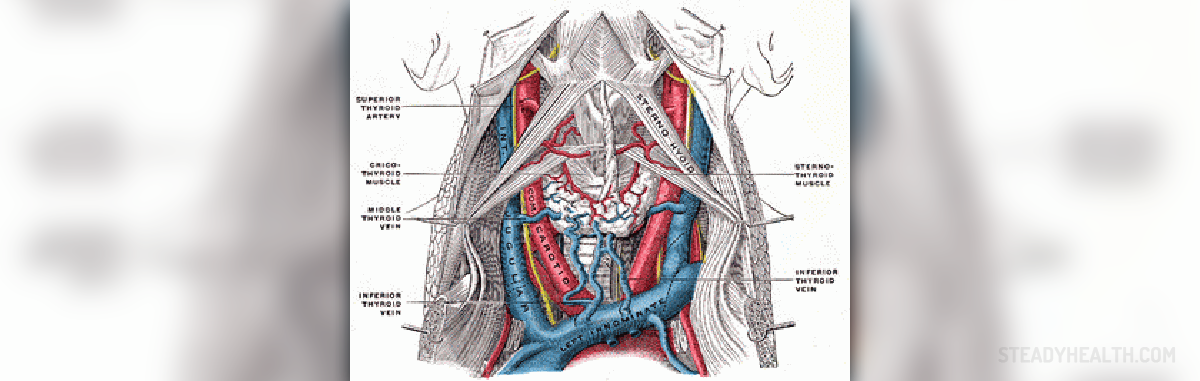
Possible causes of internal jugular vein thrombosis
The presence of central venous catheter, also known as Swan-Ganz catheter, carries a huge risk of developing jugular thrombosis. Even if this catheter is inserted into the subclavian vein, it can lead to thrombosis of the internal jugular vein.
Lemierre's syndrome can be presented with thrombosis of this vein. Infections of deep neck tissues and necrosis of soft tissue near the vein can lead to its thrombosis. It can be a complication of malignant tumors present in the head and neck.
Thrombosis of the internal jugular vein can also occur after neck dissection surgery. Increased coagulation can be present in numerous medical conditions, including different malignant tumors and problems regarding factors of coagulation. In this case hypercoagulation can also lead to thrombosis of internal jugular vein. And finally, this condition may be a consequence of jugular region trauma.
Symptoms of internal jugular vein thrombosis
The delicacy of the symptoms of internal jugular vein thrombosis may often confuse doctors. The diagnosis, therefore, can be easily overlooked, and coming to the correct conclusion requires a doctor who is committed to figuring out the mystery of the patient's symptoms, along with an X-ray.
Common symptoms of internal jugular vein thrombosis are pain and edema at the angle of the jaw. However, they may not be visible. This is why the doctor has to palpate the jugular area and he or she may feel the lump or cord under the sternocleicomastoid muscle. Still, even this change may not be palpable, which only makes the setting of the definitive diagnosis harder.
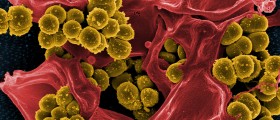
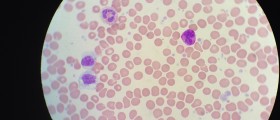
Additional symptoms of internal jugular vein thrombosis that are present in many patients include increased body temperature and an increased number of white blood cells. Most of the patients do complain about the pain in jugular area. Luckily, the mass is visible in almost 72% of all patients. Patients may suffer from shortness of breath, as well.
Some patients develop sepsis and this can lead the doctors to consider possible thrombosis of internal jugular vein. Pulmonary embolism may be the first sign of the condition. A small number of patients develop superior vena cava syndrome or jugular foramen syndrome. And in extreme cases chylothorax can occur.
All in all, the sooner the doctors set the correct diagnosis, the better is the outcome of internal jugular vein thrombosis.











Your thoughts on this
Loading...