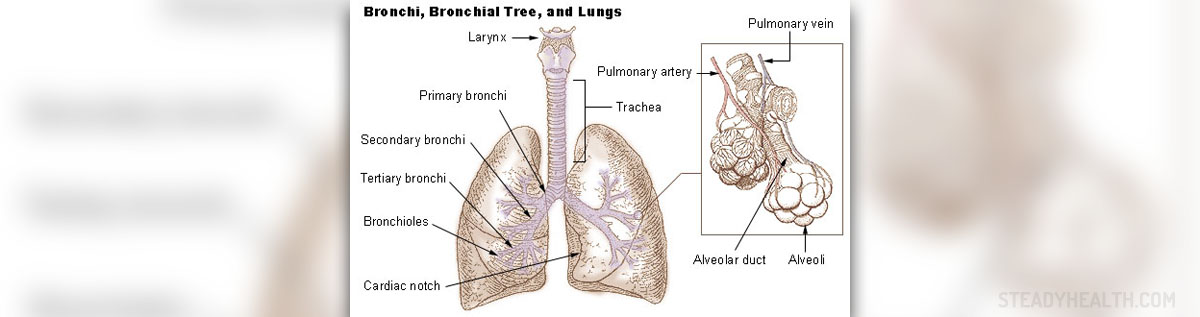
Pulmonary vascular disease is the term medical experts use for a range of conditions all of which affect the blood vessels in the lungs.
Respiratory Problems Caused by Vascular Disease
In case of pulmonary vascular disease all the symptoms and signs develop as a consequence of damage to the blood vessels that are located between the heart and the lungs. The blood delivered to the lungs is rich in carbon dioxide and after this gas is released and the blood enriched with oxygen it leaves the lungs and re-enters the heart, ready to be distributed across the entire body.
Any damage to blood vessels that are in charge with transfer of blood from the heart to the lungs and back to the heart once again is a cause of pulmonary vascular disease. There are several condition that belong to this group of illnesses. They include pulmonary arterial hypertension, pulmonary venous hypertension, pulmonary embolism and chronic thromboembolic disease.
Symptoms and signs patients suffering from pulmonary vascular disease experience basically depend on the type of damaged blood vessels, disease progression and the percent of the vascular system affected by the disease. Pulmonary Embolism is One of the most Common Issues
In patients suffering from pulmonary embolism there is a blood clot or multiple blood clots blocking blood vessels in the lungs. These form somewhere else in the body and travel to the lungs. Large blood clots cause obstruction of blood vessels with large diameter such as the main artery of the lungs while smaller ones easily pass this blood vessel blocking smaller blood vessels and causing less severe form of the disease. In the majority of cases blood clots that trigger blockage originate from deep veins of the lower extremities.
Furthermore, it is also possible to develop pulmonary embolism due to embolisation of air, fat, amniotic fluid or talc in drugs injected by intravenous drug users.
Proximal leg deep venous thrombosis, however, remains the leading cause of pulmonary embolism. It is estimated that in around 15% of all patients suffering from deep vein thrombosis the blood clot dislodges and moves towards the lungs. Changes in blood flow, changes in the vessel wall as well as factors affecting the quality of circulating blood determine whether the blood clot will develop in the first place and if it will eventually dislodge and migrate to other parts of the circulatory systems. The risk of venous thrombosis and subsequent pulmonary embolism is higher in people who are immobilized for a long period of time (especially after surgery, injury etc.), pregnant women, obese individuals and people suffering from certain types of cancer. Increased susceptibility to blood formation is also reported to occur in women using estrogen-containing contraception and patients suffering from genetic or acquired thrombophilia.
When it comes to symptoms and signs of pulmonary embolism, these include sudden onset of shortness of breath, rapid breathing and chest pain, the one that tends to become much worse when a person takes deep breaths. Cough and coughing up blood/mucus mixed with blood occur as well. Cyanosis affects patients in whom the lungs do not receive sufficient amount of oxygen and cannot release excess of carbon dioxide. Although auscultation of the lungs may be normal, sometimes there may be a pleural friction rub. What is more, auscultation may reveal pleural effusion, a collection of fluid between the parietal and visceral layers of the pleura. Patients who have additionally developed pulmonary hemorrhage/infarction may have increased body temperature. Lethal outcome is inevitable in around 15% of patients.
Diagnosis is established thanks to symptoms and signs, clinical findings and laboratory tests. Imaging studies such as CT pulmonary angiography are of additional help.How is Pulmonary Embolism Treated?
The cornerstone of treatment is anticoagulant therapy. Anticoagulants dissolve the blood clot and establish reperfusion of the affected lungs. Symptomatic and supportive treatments are applied too.
Initially, practically all patients are administered heparin or fondaparinux. After a few days patients continue taking other anticoagulants such as warfarin, acenocoumarol or phenprocoumon. During the treatment all patients are closely monitored and parameters regarding coagulation are frequently checked. The dose of the drug is always adjusted according to laboratory findings.
Treatment is administered in hospital environment while only when bodily functions are normalized patients may continue taking medications at home. Apart from treatment for pulmonary embolism it is essential to treated deep vein thrombosis as well and prevent recurrent obstruction of lung blood vessels.
Finally, prognosis of pulmonary embolism practically depends on the portion of the lungs affected by obstruction. Comorbidities make the prognosis worse. Massive pulmonary embolism easily leads to death if anticoagulants are not administered straight away. Chronic embolisation is a common trigger of pulmonary hypertension. All in all, the condition can be treated and patients saved on time. The problem is that once anticoagulant therapy is discontinued the recurrence of deep vein thrombosis and its complication - pulmonary embolism rises.













Your thoughts on this
Loading...