Jugular Vein Thrombosis - Overview
The jugular veins are part of the venous system of the body. They carry deoxygenated blood from the head back to the heart. There are two pairs of jugular veins, internal jugular veins, and external jugular veins. The internal jugular veins run next to the common carotid artery and the vagus nerve. The external jugular veins run more superficially and are located next to the sternocleidomastoid muscle. The pain which may be associated with these veins is caused by the process of thrombosis.
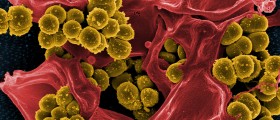
Thrombosis of the jugular veins is a serious medical condition that typically occurs as a consequence of head and neck infections, different surgeries, central venous access, local growth of malignant tumors, polycythemia, hyperhomocysteinemia, and intravenous drug abuse. Thrombosis in rather rare cases occurs spontaneously.

Jugular vein thrombosis carries a significant risk of certain complications such as death. The complications include systemic sepsis, chylothorax, papilledema, airway edema, pulmonary embolism, etc.
Setting the diagnosis of jugular vein thrombosis may be rather challenging and the doctor must be well experienced to suspect of this medical condition.
Causes of Jugular Vein Thrombosis
The leading cause of jugular vein thrombosis is the insertion of central venous catheters. One study confirmed the occurrence of jugular vein thrombosis in 66% of all patients who had undergone a central vein catheterization. The risk significantly increases if patients suffer from comorbidities and have low cardiac output. Even the insertion of a venous catheter into the subclavian vein may lead to jugular vein thrombosis.
Apart from a central venous catheter there are several more causes of jugular vein thrombosis. Namely, this medical condition typically affects people who abuse intravenous drugs and inject the drugs via the jugular vein.
Furthermore, jugular vein thrombosis affects people suffering from Lemierre syndrome, deep neck infections, and necrotizing soft tissue infections. It may also be a consequence of neck dissection surgery and occurs due to the presence of malignant tumors of the head and neck. Even distant malignant disease may induce hypercoagulation of the blood which eventually leads to jugular vein thrombosis.
Apart from hypercoagulation any kind of trauma to the jugular vein may result in thrombosis. And hyperhomocysteinemia, polycythemia, as well as a neck massage, may be several more causes of jugular vein thrombosis. Even though it happens rarely in some people thrombosis may occur spontaneously.
No matter what the cause of jugular vein thrombosis is, this medical condition requires prompt medical care and hospitalization. The treatment of thrombosis is conservative or surgical depending on the underlying cause.
- The inclusion criteria were as follows: (1) studies reporting patients with an objective diagnosis of IJVthr; (2) studies correctly addressing the question of the search reported in the abstract; (3) studies reporting the related clinical outcome. Studies satisfying all the inclusion criteria were selected.
- Using the predefined search strategy, 1490 titles were retrieved and scanned. Data from randomized control trials were few and limited to the central vein catheterization route and material and to the IJVthr anticoagulation treatment. No systematic reviews were available, except for Lemierre syndrome and IJVthr, and jugular thrombosis following catheterization.
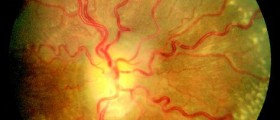
- There were several common clinical signs. The most frequent were neck swelling and erythema and the palpable cord beneath the sternocleidomastoid muscle, frequently associated with fever. Oedematous swelling of the face/scalp, papilledema, and intracranial hypertension were also reported in several papers. These kinds of symptoms could be ascribed to a possible impairment of the cerebrospinal fluid dynamics, which is strictly connected to the cerebral venous outflow.
- Laboratory results showed the D-dimer raising and leukocytosis were the most common abnormalities. Quite recently, a number of papers focused on symptoms related to IJV obstruction, especially from bone and muscular compression but even from kinking of the carotid arteries. IJV obstruction from bone nutcracker represents a risk factor for the development of IJVthr.
- The most recent one on 5039 autoptic cases collected in several German hospitals, deep vein thrombosis (DVT) was found in 1725 cases (34.9%). In 404 cases it was found in the superior vena cava system, in 730 cases in the inferior vena cava system, and in 248 cases in combined localization. Pulmonary dissection revealed embolism in 1500 cases (29.8%), of which it was fatal in 628 cases (41.9%). In 12.6% the thrombosis was present in the upper system while in the lower extremity was found 5 times (59.4%) more common. Interestingly, after the routinely introduction of the central veins’ catheterization, the location of DVT was found in the right IJV in 30.9%, in the left IJV in 15.7%, in the left femoral vein in 32.7%, in the right femoral vein in 30% and in the deep calf veins in 15.1%.
- The conservative treatment of IJVthr not complicated by CVT (thrombosis of the cerebral veins) is not different from the anticoagulation regimen and duration recommended for deep vein thrombosis in the lower limbs and PE. Management of catheter-related venous thrombosis varies and is not well established, yet. If the catheter can be removed, and there is a low risk of embolization and no prothrombotic risk, the catheter should be removed, and there is no need for anticoagulation therapy. If there is a high risk of embolization, anticoagulant therapy should be initiated.














Your thoughts on this
Loading...