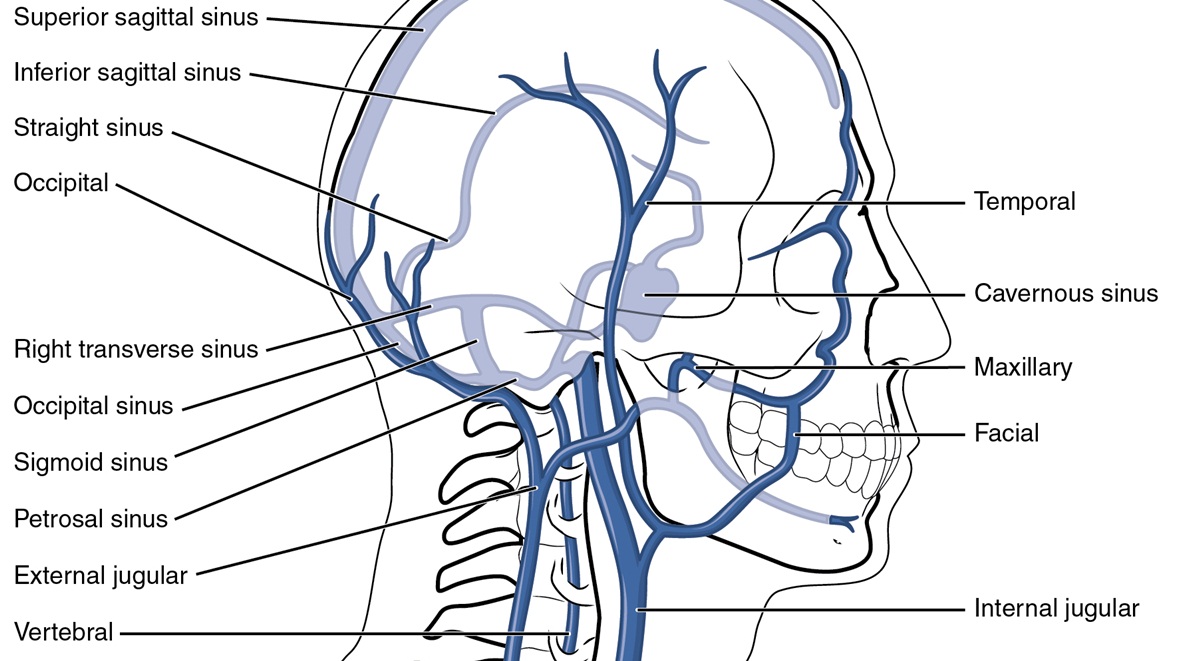
Jugular Vein Thrombosis Overview
Thrombosis of the internal jugular (IJ) is a rare but under-diagnosed condition. Jungular vein thrombosis is most commonly caused by cancer, central venous catheter, and the ovarian hyperstimulation syndrome related to some fertility treatments. Thrombosis of the internal jungular vein can occur as a result of complications of head and neck infections, or sometimes related to surgeries, central venous access, local malignancies, or intravenous drug abuse.
- The tunica adventitia, or the outermost layer of the vein's wall, is the thickest of all layers. It is composed of loose connective tissue that connects to other tissues in the body.
- The tunica media, or middle layer, is made up of collagen, elastic fibers, and smooth muscle.
- The tunica intima, or innermost layer, is the thinnest layer of the vein’s wall, and is composed of an internal elastic membrane and connective tissue.
Sometimes, however, it can even occur spontaneously.
It is important to identify the problem early because IJ thrombosis can have very serious and potentially life threatening complications, including systemic sepsis, chylothorax, papilledema, airway edema, and pulmonary embolism.
It is essential to see a doctor because the diagnosis is very hard to pin down and it requires a very serious and high degree and level of expert clinical suspicion. The symptoms typically associated with thrombosis of the internal jugular are neck pain and swelling of the surrounding lymph nodes.
The Infection of Thrombosis
The thrombosis can also become infected secondarily and result in septic thrombophlebitis.
Studies that have been done regarding these conditions suggest that the rate of the thrombosis can be lower for silastic hemodialysis catheters that are percutaneously inserted, in comparison to those that are implanted through surgery.
Sometimes the infection occurs as a result of Lemierre syndrome, a possible complication of pharyngeal infections. Thankfully, since the introduction of antibiotics in the late 1950s, occurrences of Lemierre syndrome have fallen quite drastically.
There are no figures that give detailed statistics on the frequency of IJ thrombosis in people who are intravenous drug users, but it does occur quite commonly for people who have been injecting drugs into their veins for many years and have exhausted many of the veins commonly used.
Thrombosis of the Internal Jugular Treatment
Once thrombosis of the internal jugular is diagnosed, the use of an anticoagulant therapy is what is commonly recommended.
However, there are no studies that are reliable enough regarding this treatment, and even treatment recommendations are controversial. But, the fact that the condition is severely under-diagnosed also points to the fact that many patients will do well without serious effects.
There is a risk of pulmonary embolisms, but this too is under-researched.
In most cases of IJ thrombosis, a prolonged antibiotic therapy is commonly recommended to work against the anaerobic organisms as soon as the blood cultures are obtained. The duration of the antibiotic treatment is usually in between four and six weeks.
In some cases surgery is needed, but seldom in uncomplicated ones.
However, when there are deep neck infections that require drainage of fluid collections and a debridement of the infected tissue, then a surgery will be mandatory.
A case of intraluminal abscesses could also require the IJ vein to be excised so that the doctors can prevent greater and more serious damage to the area. Your healthcare provider will decide the right treatment for your particular cases after weighing all the options, should you be diagnosed with thrombosis of the internal jugular.
Usually surgery is not needed because there are very few cases of IJ thrombosis that cannot be treated with the right antibiotic therapy, often anticoagulant therapy that lasts up to a month, and even non-steroidal anti-inflammatory medications can be prescribed in these cases of thrombosis of the internal jugular. In many cases, fevers will occur, especially in cases of metastatic infection.








-Arthritis_f_280x120.jpg)




Your thoughts on this
Loading...