Total parenteral nutrition -TPN or hyperalimentation, is the practice of feeding a person, but not via mouth but blood. It is normally used during surgical procedures. It has been used for patients in a coma although enteric (tube) feeding is adequate and effective because it is less complicated. Chronic TPN is used to treat patients suffering from an accident or a complicated surgery. In the TPN's simplest way, a bag of liquid nutrients is added to a patient's intravenous drip.
The intravenous injection of nutrients is called parenteral feeding. It can be given to a patient orally or via tube intravenously, and this type of nutrition is called parenteral nutrition. Patients who are malnourished, at risk of being like that, or with an unreachable gastrointestinal tract need an intravenous injection of nutrients.
The access on the skin can not be used for anything but injecting nutrients. The solution for parenteral nutrition is thrombogenic and conducted like a vein irritant. Parenteral feeding is actually direct access and provides the concentrated formula to flow into main vessels.
A peripherally expectorate central catheter (PICC) is done with an aseptic technique. Intravenous feeds of low osmolality and neutral pH are ascent. TPN solutions are manufactured in sterile condition in plastic sterile 3-liter bags.
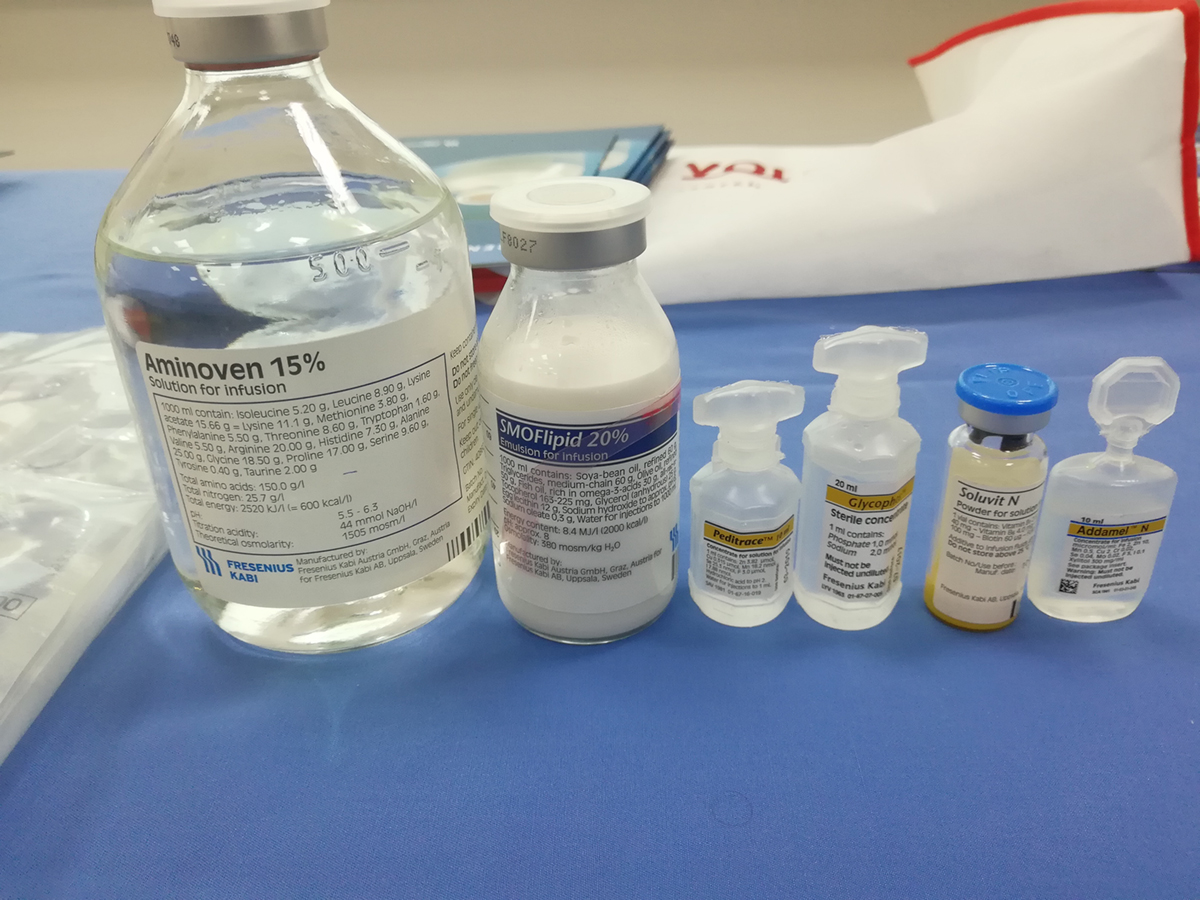
TPN solutions are injected intravenously and have the right mixture of essential and non-essential amino acids micronutrients glucose fat and electrolytes. The solution is iso-osmotic lipid emulsions, an energy solution that also alleviates vein irritation. The solution also has a small concentration of glucose that inhibits hyperosmolar dehydration.
The way parenteral nutrition is given to patients is gradual, at a continuous flow rate. The solution contains folic acid with vitamin B12 given separately from the injection.
The Complications - Re-feeding Syndrome
The complications may occur with hypophosphataemia, along with electrolyte disturbances due to a solution-feeding stimulation of the cellular electrolytes. It takes about 4 days of re-feeding for clinical features to thrive. And later on, that may cause hypotension, rhabdomyolysis, seizures, respiratory failure, cardiac failure, arrhythmias, and coma.
Catheter Complications
The instantaneous complications are pneumothorax, haemothorax, cardiac tamponade arrhythmias, and hemorrhage. Catheter complications are long termed and are venopulmonary fistula, subacute bacterial endocarditis, chylothorax, pulmonary embolism pleural pericardial effusion, and thrombosis.
Possible Infection
Infections due to parenteral feeding are septicaemia (that may end with death because of the catheter-related sepsis) enterococci and staphylococcal species. Also, there is liver and gallbladder failure and slugging of the gallbladder, and gallstones.
- Central venous catheters, both short-term and long-term, are associated with infectious complications.
- Other than central line infections, parenteral nutrition (PN) increases the overall risk of infection, including pneumonia and intra-abdominal abscess. A meta-analysis by Elke et al. on 18 RCTs including 3347 patients compared the clinical outcomes of enteral and parenteral nutrition in critical care patients. EN showed a significant reduction in the rate of infection compared to PN, but this effect was only seen in a subgroup of patients where the PN group received a significantly higher caloric intake.
- Global guidelines for the prevention of intravascular catheter-related infections emphasize the importance of educational programs for healthcare workers and patients regarding infection protection and hand decontamination.
- Other efforts are being investigated to further reduce infection complications, such as chlorhexidine-impregnated dressings, which is now also a part of recent global guidelines. In an RCT by Wouters et al. comparing taurolidine locks to 0.9% saline locks, a significant reduction in catheter-related bloodstream infections were shown in patients with newly inserted central catheters.
Hyperglycemia
Hyperglycemic patients have to get nutritional addictions, in which case glycemic control is absolutely necessary also a treatment with insulin and oral hypoglycemic agents is needed.
















Your thoughts on this
Loading...