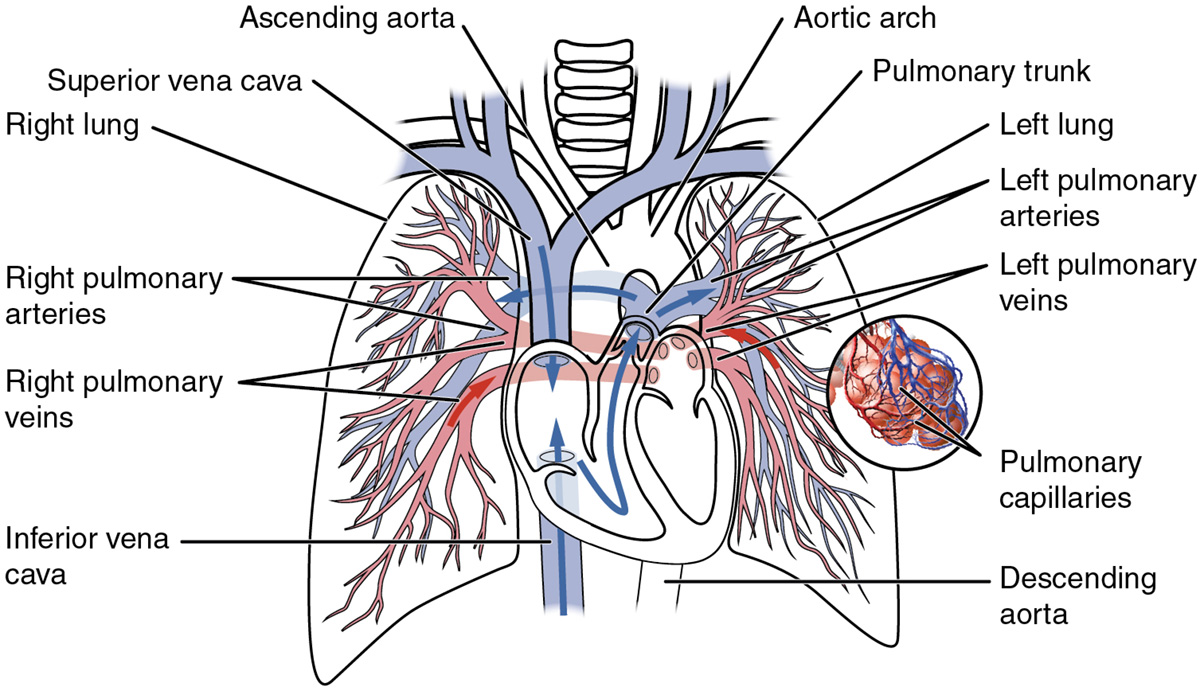
Pulmonary embolism is a blockage of the pulmonary artery or its smaller branches due to dislocation of a blood clot (thrombus) or other bodies from the periphery, through which they enter in the pulmonary blood circulation. Embolism can cause blood clots, fat droplets, gases, foreign bodies, bacteria, parasites and the body cells.
The most common cause of pulmonary embolism is a thromboembolism in the deep veins of the lower extremities and pelvis. Thrombi can rarely come from the heart, if it is expanded or from superior vena cava.
Risk factors for a venous thrombosis of lower extremities are usually prolonged sitting and lying after surgery, tumors, blood coagulation disorders etc. Thrombi which are separated from their primary position carried by the blood may block pulmonary artery. Obturation of pulmonary artery causes a sudden increase of resistance and pressure in the pulmonary circulation leading to loading the right ventricle of the heart. If the load is large, the heart can not deflate enough blood which is known as cardiogenic shock.
Most pulmonary embolisms pass without symptoms, because small arteries are mostly closed. Obstruction of small branches of pulmonary arteries leads to infarction of the lungs, or the extinction of small segments of the lungs. However, if the affected area receives an additional circulation from the surrounding arteries it does not cause pulmonary infarction, but appears pulmonary hemorrhage.
If there is a blockage of the main pulmonary artery it performs immediate death. If the patient survives massive embolism, develops the heavy shock. Later appears difficult dyspnea (difficulties with breathing), the patient is very frightened, he/she has pain behind the sternum and cold sweating. Also develops pale cyanosis, blood pressure decreases, pulse is rapid, veins in the neck are swollen and liver gradually increases. If pulmonary embolism is less, the patient has a mild and short-term dyspnea, he/she is anxious, suddenly sweating, has tachycardia, has a moderate fever and primary disease worsens. Symptoms of pulmonary infarction occur 12-48 hours after pulmonary embolism. Suddenly appears pleural pain localized in the lower parts of the lungs. Pain can be projected to the neck or upper part of abdomen. Other symptoms include persistent cough, coughing up ichor, shortness of breath (dyspnea), tachycardia, fever, sometimes mild jaundice. Laboratory test show increased white blood cell count, sedimentation, bilirubin, and lactic acid dehydrogenase levels in the blood. The x-ray shows a characteristic triangular shadow and irregular or round shadow like at bronchopneumonia.
With early diagnosis and aggressive treatment, most patients will survive pulmonary embolism with low rate of recurrence.
The use of oxygen by mask or nasal catheter mostly helps patients, but for those with very high hypoxia tracheal intubation and mechanical ventilation are necessary. Hypotension, or cardiac failure, usually requires using inotropic agents and vasopressors.
Thrombolytic therapy (blood clot breakdown) is the main therapeutic measure. It carries out with streptokinase, urokinase and tissue plasminogen activator. It shouldn’t be applied in situations where bleeding may occur (pregnancy, internal bleeding in the last two months, injury or surgery in the last ten days and malignant hypertension).
Then anticoagulant therapy applies, which is conducted by infusion of heparin or anticoagulants in tablet form (Farin, Pelentan etc.). Antiplatelet therapy (prevention of thrombosis) is usually conducted by taking Aspirin. Bronchodilators and antibiotic also uses. Surgical treatment has traditionally been reserved for patients with massive pulmonary embolism and cardiac collapse.














Your thoughts on this
Loading...