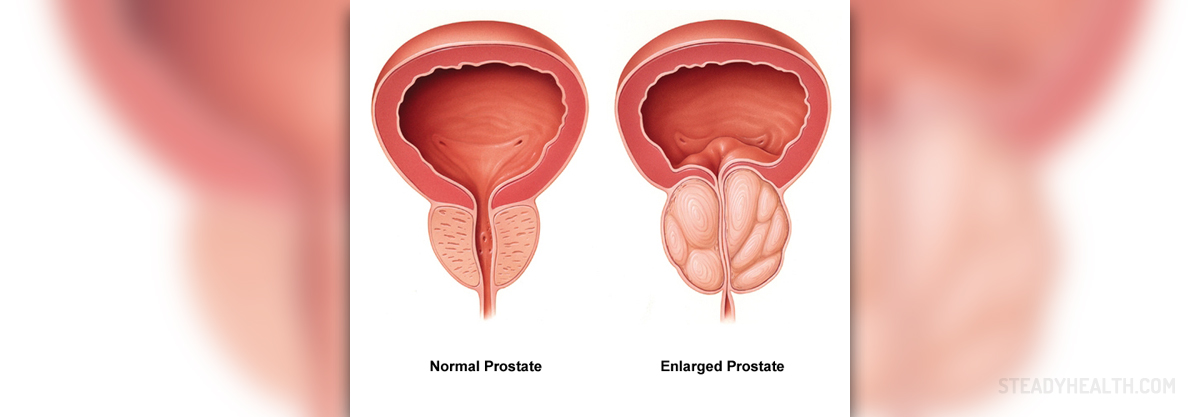
The prostate is a gland placed below the bladder, and a part of the urinary tube passes through it. Only men have the prostate. Its role is still incompletely tested, but it is known that this gland produces a liquid part of semen. It has the same size as a chestnut and begins to grow immediately after the age of 25.
Symptoms
Prostate enlargement is the consequence of the male sex hormone – testosterone (dihydrotestosterone). Somewhere around the age of 50, a man begins to feel symptoms of enlarged prostate. They are manifested in frequent nocturnal enuresis, slowed or delayed urination, weak urine flow, inability to delay urination, incomplete bladder emptying, the abruptness of urine flow during bladder emptying, urine dripping, which takes a few seconds at the end of urination, urination accompanied with pain, hematuria - the presence of blood in urine, urine retention, frequent urination, strong and sudden urge to urinate, incontinence - uncontrolled urination. Symptoms appear gradually, and a patient goes to the doctor only when these symptoms begin to disrupt normal life.
Treatment
Once the diagnosis is established, the enlarged prostate treatment may begin. Treatment can be:
(1) hormonal – a group of drugs that blocks alfa1 adrenoceptor (floma x, x atral, Cardura, etc.) and drugs that inhibit 5 alpha-reductase, an enzyme that is located in the prostate and is responsible for prostate growth (Proscar, Avodart). These drugs do not reduce prostate but mitigate the above symptoms of enlarged prostate.
(2) invasive - microwaves, laser, or Cryotherapy (freezing).
(3) surgical - through the urinary tube by Transurethral resection (TUR), or, if a prostate is very large, doctors perform the open surgery, in which the entire prostate is removed.
It is believed that Transurethral resection (TUR) is the gold standard in the treatment of enlarged prostate. Surgery is usually indicated in men with symptoms of incontinence, blood in the urine, urine retention, and recurrent urinary tract infections.
- Transurethral resection of the prostate (TURP) is the gold standard surgical procedure, but other alternatives using laser (HoLEP and ThuLEP) and robotic water jets (Aquablation) are emerging treatments aimed at reducing postoperative morbidity.
- Minimally invasive procedures conducted in outpatient settings and under local anesthesia or sedation are increasingly being used, especially in those patients with high surgical risk due to comorbidities. These procedures include prostatic arterial embolization, water vapor thermal therapy (Rezum), prostatic urethral lift (Urolift), temporary implantable nitinol device (TIND/iTIND), and transurethral microwave thermotherapy (TUMT).
- For those with moderate symptoms, alpha-blockers are the first treatment option, reducing symptoms by 30–40% and improving urinary flow by 20–25%. Common side effects include hypotension and ejaculatory dysfunction. However, 5-alpha reductase inhibitors (5-ARI) can cause a moderate reduction in symptoms (15–30%) and prostate size, reducing the risk of AUR and the need for surgery, but there is a latency for this improvement (3–6 months), and they are most effective in patients with larger prostates (>30 cc) that will be treated on a long-term basis.
Complications of surgical treatment are very rare, sharing the same risk with all other surgical procedures. Open prostatectomy is usually performed with general or spinal anesthesia. This procedure is time-consuming and requires staying in the hospital for seven to ten days.
American doctors are experimenting with a new and appears to be an effective method of enlarged prostate treatment with laser. Strongly focused green laser light could be a solution for common health problems among older men. Excess tissue, which causes urological disorders, is removed by simple surgery thanks to this device.
The surgery has no side effects, which normally occur in conventional prostate surgery. The procedure is done outpatient, and patients can be released from the hospital on the same day. Laser light is so strong that surgeons and nurses have to wear special protective glasses.
This procedure is particularly suitable for patients who don't feel any improvement after drug therapy, and for those who for some reason cannot or do not want to undergo traditional surgery with a scalpel. The surgery is so precise that the removal of tissue doesn't affect the surrounding nerves and other sensitive cells.
















Your thoughts on this
Loading...