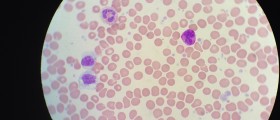
Mantle cell lymphoma, also known as simply MCL, is one of the rarest occurring types of non-Hodgkin's lymphomas. The non-Hodgkin's lymphoma is a group of blood cancers that include any kind of lymphoma except Hodgkin's lymphomas. Lymphoma is defined as a cancer in the white blood cells of the immune system. The malignant cells are often present in the lymph nodes, and they appear as an enlargement. Mantle cell lymphoma is a rare disease that comprises about 6% of all non-Hodgkin's lymphomas. It is estimated that currently only 15.000 patients in the United States suffer from mantle cell lymphoma.

Lymphomas
Human body is covered with small lymph nodes. These nodes serve as body’s filters for everything that is harmful: bacteria, viruses, damaged cells and cancer cells. As the lymph fluid flows through the body, it picks up and carries away this waste. Lymph contains white blood cells called lymphocytes, which are critical for body’s defense against infections and diseases.
Most of these cells originate from bone marrow: B-cells completely develop in the bone marrow, while T-cells go to the thymus gland to mature before being released into the rest of the body. In lymphoma, these cells grow in an uncontrolled way, and the lymphatic system enlarges before it stops working properly. Mantle cell lymphoma is a cancer of the B-cells that usually starts at any age from the late 30s to old age.
Symptoms and causes of mantle cell lymphoma
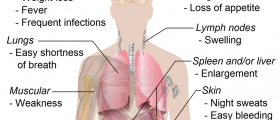
In most of the cases, patients will have symptoms of fever, heavy night sweats and unexplained weight loss. The lymph nodes (in the underarms, groin, neck, chest and abdomen) and the spleen will typically become swollen. The patients typically notice a “bump” on the neck or in the armpits or groin. If the lymphoma affects the bowel or stomach, it can cause symptoms such as diarrhea or sickness. Causes of mantle cell lymphoma are yet unknown. In most of the cases, doctors suspect exposure to toxins.
Prognosis and treatment
The 5-year survival rate for mantle cell lymphoma is generally 50%, for advanced stage, to 70%, for limited-stage mantle cell lymphoma. There is no absolutely successful treatment for this disease. It seems like most of the patients shortly benefit from chemotherapy, but their condition typically progresses after this treatment. The relapse episodes are usually more difficult and there is no way, at the present, to treat relapse. Commonly used treatments include chemotherapy, immune based therapy, radio immunotherapy and new biologic agents.
Active treatment is started if the patient begins to develop MCL-related symptoms or there are signs that the disease is progressing. MCL is usually diagnosed once it has spread throughout the body, and the majority of patients ultimately will require treatment
- Initial treatment approaches for MCL in younger patients include the monoclonal antibody, rituximab (Rituxan), with a cytarabine (Cytosar)-containing combination chemotherapy regimen, and are often followed by consolidation with autologous stem cell transplantation (patient’s own cells are infused after high-dose chemotherapy). This treatment may be followed by an extended course of rituximab (Rituxan) alone, known as maintenance therapy, with the goal of prolonging remissions (disappearance of signs and symptoms).
- For older or less fit patients, less-intensive chemotherapy is often recommended and may also be followed by rituximab (Rituxan) maintenance. One such treatment is bendamustine (Treanda) in combination with rituximab (BR) as a frontline (initial) therapy.
- Allogeneic stem cell transplantation (patients receive stem cells from a donor) can produce deep responses, including cure, but can also cause significant side effects. Typically, it is only used in selected younger patients whose disease has relapsed (returned after treatment).
- Bortezomib (Velcade) is approved by the U.S. Food and Drug Administration (FDA) for the treatment of patients with MCL. Studies with bortezomib (Velcade) show that the drug may be effectively combined with conventional chemotherapy.
- Lenalidomide (Revlimid) is another treatment for MCL approved by the FDA for patients who have relapsed or progressed after two prior therapies, one of which included bortezomib (Velcade). In addition to directly targeting MCL cells, lenalidomide (Revlimid) affects the growth and survival of tumor cells by altering the body’s immune cells. It may be given in combination with rituximab (Rituxan).
- Ibrutinib (Imbruvica), zanubrutinib (Brukinsa), and acalabrutinib (Calquence) are Bruton tyrosine kinase (BTK) inhibitors that stop signals in cancer cells responsible for growth and survival. All three are approved by the FDA for treatment of MCL in patients who have received at least one prior therapy.













Your thoughts on this
Loading...