Anal fissure is a condition commonly affecting both men and women, especially individuals older than 20 and younger than 40. Usually, this condition is mistaken for hemorrhoids, due to similar symptoms these two condition manifest through. However, the two are not the same and have distinctive features. An anal fissure is located either at the rear of the anus or at the front.
Types of Anal Fissures
If an anal fissure is present for less than six weeks, during which it heals, the condition is considered to be acute. However, if it remains prevalent even after this period, the anal fissure is referred to as chronic.
Acute occurrences of this problem are easily treatable and many times they go away on their own. On the other hand, chronic anal fissure bothers a person over a longer period of time, not necessarily escalating or getting worse.
Manifestations of Anal Fissure
Sharp burning or searing pain appearing around your anus is a common sign of an anal fissure, especially when it affects you immediately after a bowel movement. The pain may remain prevalent for more than a couple of hours, becoming more painful. Drops of blood may appear on the toilet paper or the toilet bowl itself. Finally, a sentinel pile may form on the edge of the anus, right below the fissure, having nothing to do with hemorrhoids whatsoever.
If you notice any of the above mentioned symptoms, seek medical assistance as soon as possible.
When an anal fissure fails to heal, it becomes chronic. Then, the tear extends into the ring of an anal muscle involved in the closing procedure of your anus. Once this happens, the pain from the fissure may trigger a spasm in the muscle, closing the anus, making the whole bowel movement process even more complicated. Yet, people should not strain themselves during bowel movements, especially if they suffer from anal fissures, since this can only make matters worse.
Causes and Treatment for Anal Fissure
Constipation and overstraining during the process of passing stool can damage your anal area, leading to anal fissure formation. Chronic diarrhea may have the same effect. Additionally, Crohn's disease, STDs, the third trimester of pregnancy, labor, diabetes, HIV or certain medications, all may lead to creation of an anal fissure.
The treatment may involve consuming foods rich in fiber and having a balanced diet altogether, preventing dehydration by consuming plenty of water and exercising regularly, promoting overall health and well-being, bettering your digestive processes.
If these steps fail, your doctor may treat this problem with certain medications or schedule a surgery which will relieve the pressure in your anal area, preventing the anal muscle from contracting during bowel movements.
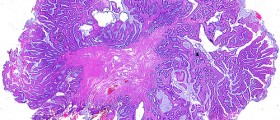
- There have been changes to the hypothesis of the development of anal fissures over the years. The initial hypothesis was that of anal canal trauma, most commonly by the passage of hard stools or bouts of diarrhoea. However, this only accounted for acute fissures but not the progression to chronic non-healing anal fissures even after the bowel consistency had improved.
- The current understanding is that there is an initiating trauma to the anal canal caused by the passage of hard stools or diarrhoea episodes. In susceptible individuals with internal sphincter hypertonia, there is little or no healing of the anal mucosa after the initial trauma. This is due to ischemia of the tissues around the anal fissure, especially the posterior commissure, by compression of the inferior rectal arteries from the internal sphincter. The paucity of blood flow prevents healing of the anal fissure until the cycle of internal sphincter hypertonia and decreased blood flow is broken by muscle relaxants or surgery.
- Conventional pharmacological treatment involves the use of muscle relaxants, commonly topical and occasionally oral agents. These agents include nitrates [ISDN or glyceryl trinitrate (GTN)], calcium channel blockers, Botulinum toxin, ?-adrenoreceptor antagonists, ?-adrenoreceptor agonists and muscarinic agonists. Newer pharmacological agents being tested include Gonyautoxin, a paralytic neurotoxin derived from shellfish.
- Conventional surgical therapy involves finger anal dilatation and lateral internal sphincterotomy. Finger anal dilatation is generally regarded by many colorectal surgeons to be an obsolete method as finger dilatation has been associated with the development of anal incontinence. Lateral sphincterotomy has been regarded as the gold standard for treatment of chronic fissures.
- Newer surgical therapies that have evolved include local flap procedures such as V-Y advancement flaps and rotation flaps. Attempts at fissure revision have lead to the development of fissurectomy and fissurotomy procedures. New interest in the technique of anal dilatation has lead to the development of calibrated and controlled procedures with anal dilatators or pneumatic balloons. A new method of blunt division of internal sphincter fibers termed sphincterolyis has also been attempted.
- One recent study looked into the use of a posterior perineal support device incorporated into a toilet seat to improve the healing rates of chronic anal fissures. This posterior perineal support device is likely to reverse the preferential over-stretching of the posterior anal sphincter complex and mucosa and thus facilitate defaecation with less trauma. This study on 32 patients with symptomatic chronic anal fissures reported: at least moderate (or greater) improvement in pain for 50% of patients at 2 weeks with 97.5% improvement at 3 months. The improvement in pain was also manifested in a decrease in pain score from five (before treatment) to zero (at 3 months).
















Your thoughts on this
Loading...