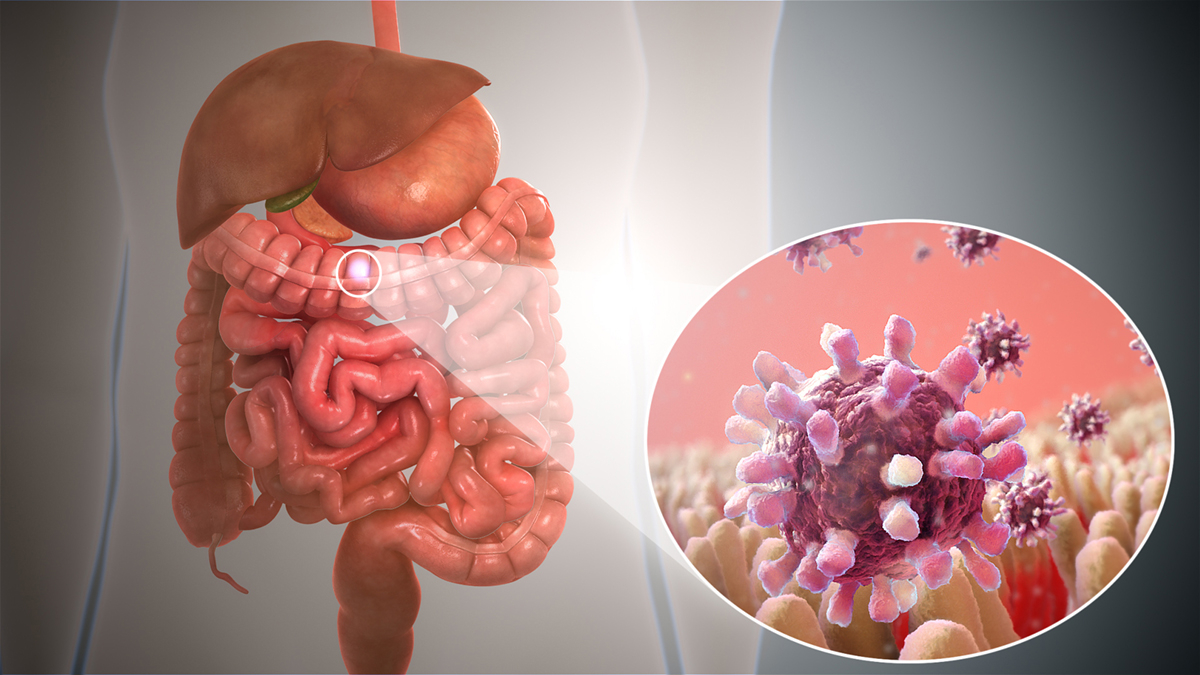
Pathogens in Bowel Infection
There are a lot of causes of intestinal infection, such as bacteria, viruses, yeast, mold, parasites, fungus, or simply unhygienic conditions. Each of these organisms is a pathogen, and it can infect any part of the human body, but the most common body part they infect is the gastrointestinal tract.
If untreated, this kind of infection can lead to death, but the level of risk depends on the type of the pathogen causing the infection in the first place. The two most common causes of infections of the gastrointestinal tract are poor hygiene of the person infected and pathogens in the food the person eats. Another common cause is shellfish, and people who eat shellfish should know that if not cooked well, pathogens from the shellfish will find their way to their stomachs.
Cramps are the most common symptom of intestinal infection and can be very severe. Cramps usually last for three to four minutes. Constant abdominal pain is another common symptom of an intestinal infection, especially if it lasts for a prolonged period.
A person should see a doctor if he or she experiences this problem. Nausea is commonly experienced along with cramps. It is not uncommon for a person who is affected to feel disgust toward food. However, if this loss of appetite continues for a prolonged period, a person should consult a doctor. Diarrhea is another common symptom of an intestinal infection, and since it causes dehydration, it is very important to take enough fluids and consult a doctor.
- Multiple studies have reported GI symptoms in COVID-19 patients, including diarrhea, nausea, vomiting, anorexia, and abdominal pain. According to a meta-analysis comprising 10,890 COVID-19 patients, the pooled prevalence estimates of GI symptoms were: diarrhea (7.7%), nausea or vomiting (7.8%), and abdominal pain (2.7%) with 10% of these patients reporting GI symptoms as being their initial symptoms.
- With the deepening understanding of COVID-19, GI symptoms have been recognized as early signs of the disease. The high expression of ACE2 in the GI tract, isolation of live virus from fecal samples, and a subset of patients presenting with only GI symptoms seem to suggest fecal–oral transmission. However, problems with the feasibility of this mode of transmission remain. First, studies have shown that SARS-CoV-2 loses infectivity in simulated gastric acid within 10?min.
- Secondly, SARS-CoV-2, as an enveloped virus, is largely unable to withstand the detergent effect of bile salts and the activity of digestive enzymes in the duodenum. Although some studies have suggested that highly viscous mucus in the gastrointestinal tract protects SARS-CoV-2, allowing the virus to retain its infectivity, there is still a lack of direct evidence.
- A recent study has shown that a fecal sample positive for SARS-CoV-2 RNA at any time during hospitalization was associated with higher mortality [HR: 3.4 (1.2–9.9)]. Similarly, another study showed that small-bowel thickening on CT was strongly associated with ICU admission. This relationship did not hold for colon or rectal thickening. These data indicates that small-bowel damage contributes to poor outcomes. As the main organ for nutrient absorption, damage to the small intestine will result in malabsorption and malnutrition, both of which commonly occur in COVID-19 patients.
- Intestinal ischemia is a common manifestation in COVID-19 patients. Autopsy results have shown that 31.6% of deceased patients had focal ischemic intestinal changes. In a separate imaging study, bowel wall thickening and pneumatosis intestinalis, which indicate intestinal ischemia, were found on 38.1% (16 of 42) of abdominal CT images. Of these, 4 (9.5%) patients with pneumatosis intestinalis developed severe intestinal necrosis and needed resection. In another cohort study, 55.8% (58/104) of ICU patients developed an ileus.
- Long-term GI complications are common in recovering COVID-19 patients. In one systematic review of post-acute COVID-19 manifestations, diarrhea was among the top 10 most common complaints, with a prevalence of 6%. Other long-term GI symptoms include nausea, vomiting, abdominal pain, loss of appetite, and weight loss.
Apart from these, constipation, irritable bowel syndrome, and problems with sleeping are common symptoms as well. The symptoms must be treated on time for certain complications to be avoided. In case of depression and headaches, a person should see a doctor as soon as possible.
Treatment
First, a person infected should change their diet and start drinking much more fluids because of possible dehydration. One should avoid heavy foods and consume foods considered a home remedy for intestinal infection, such as ginger tea, peppermint tea, banana, and so on.
Sounds in the Bowel? A Sign of Infection?
When the food is being digested, the bowels can make some strange sounds like gurgling or outright loud rumblings that seem to come from the very depth of the stomach. Once a person has filled the stomach with a delicious meal, the body then needs to extract the nutrients from it for the benefit of the body.
As the food is processed, it passes through the intestines. During this process, abdominal sounds are generated from the stomach area. Intestinal motility or peristalsis are the sounds that come off as rushing and gurgling sensations, and the stomach can produce noises that are audible to people near the person suffering from them. These sounds and sensations of rushing are an indication that the bowels are working correctly within the gastrointestinal tract, but other sounds may be a sign of Crohn’s disease, gastroenteritis, food hypersensitivity, ulcerative colitis, and others.
Bleeding in Bowel Movement is a More Serious Condition
Bleeding during bowel movement is a condition that occurs in older people, as well as in the young population. In the majority of cases, this bowel disorder typically occurs because of bad lifestyle habits.
There are a lot of causes of bleeding in bowel movements, and it is very important to establish the real cause of it. In most cases, the causes are not serious, but certain severe medical conditions may cause this disorder, such as colon or rectum cancer. This is why it is important to determine the exact cause of the condition so that proper treatment can be immediately conducted.
Bleeding during a bowel movement may be also induced by hemorrhoids, fistulas, diverticulitis, proctitis and colitis, rectal fissures, and protrusion of the rectum. Hemorrhoids occur because of excessive pressure on the walls of the rectum, which causes swelling of the blood vessels in the rectal or anal area. Hemorrhoids may be external or internal. The external ones can be felt while wiping. When the hemorrhoids burst, they cause bleeding, and the most common reason for the outbreak of hemorrhoids is chronic constipation. This is why hemorrhoids are a lot more common in pregnant women. The stool softeners are recommended for the treatment of this medical condition.
A person can end up suffering from bleeding during bowel movement due to the forming of fistulas from the rectum to the skin around the anus. This condition is usually treated with antibiotics or certain other types of prescription medications.
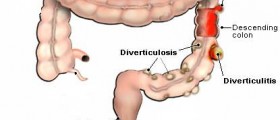
Diverticulosis is the medical term for the inflammation of the diverticula that forms in the walls of the bowel. Diverticula are tiny sacs that can burst and bleed.
The inflammation of the rectum, medically called proctitis, is also one of the causes of bleeding during bowel movement. Colitis, on the other hand, is the medical term for the inflammation of the colon, and it also may lead to bleeding.
Ulcerative colitis is a condition in which the inner surface of the colon is inflamed and full of ulcers. Chronic constipation and chronic diarrhea are also known as common causes of bleeding in bowel movements in a lot of cases.
- www.betterhealth.vic.gov.au/health/conditionsandtreatments/diverticulosis-and-diverticulitis
- www.nhs.uk/conditions/inflammatory-bowel-disease/
- Photo courtesy of https://www.scientificanimations.com/ by Wikimedia Commons: commons.wikimedia.org/wiki/File:Gastroenteritis.jpg















Your thoughts on this
Loading...