Granulomatosis with Polyangiitis, previously called Wegener's granulomatosis, is a rare member of the vasculitis umbrella. The condition leads to inflammation of blood vessels that in turn restricts blood flow, and is known to affect the nose, lungs, kidneys and certain other organs. While Granulomatosis with Polyangiitis used to be fatal in most cases, advances in modern medicine now mean that the majority of patients can go into remission, though flare-ups are a risk.
Granulomatosis with Polyangiitis: ProblemsGranulomatosis with Polyangiitis is still a life-threatening disease, though treatment with a combination of cyclophosphamide and prednisone leads to success in nine in every 10 patients. Of these, almost 50 percent will eventually suffer a relapse.
Damage to the affected organs develops as a result of the attack of autoantibodies known as anti-neutrophil cytoplasmatic antibodies (ANCAs). These antibodies trigger damage and inflammation of small and medium-size blood vessels. Symptoms and signs of the disease may occur suddenly, or develop gradually over time.
Initially, most patients complain of respiratory problems. Further progression of the disease triggers symptoms associated with damage to other organs like the kidneys. Practically all characteristics of the disease start with inflammation of certain blood vessels which subsequently affects the function of the affected organ.
First of all, damage to the mucous membrane of the nasal cavity leads to a runny nose and pus-filled discharge. Nosebleeds are also frequent. The lining of sinuses may become inflamed, which then results in chronic sinusitis.
Secondly, patients suffering from Granulomatosis with Polyangiitis have problems with their gums. These are prone to inflammation and bleeding. Their voice may become hoarse. Repeated ear infections occur too.
Additionally, the majority of patients experience respiratory issues such as cough, chest pain, hemoptysis (coughing up blood), wheezing and shortness of breath.
Weight loss, malaise, fever, joint aches and swelling as well as skin sores are several more health problems patients might face. If the eyes are affected by inflammation, they become red, start to burn, and may become very painful. Double vision or decreased vision are also possible.
And finally, hematuria is something that points to the presence of functional kidney abnormalities caused by damage to the kidneys i.e. their blood vessels. Severe loss of blood is accompanied by anemia.
All in all, the symptoms and signs can be very complex and damage to the organs quite severe, eventually triggering organ failure. Progression of the disease might be very rapid and in order to bring the condition under control doctors must think quickly and confirm the condition as soon as possible.
Biopsy to Diagnose Granulomatosis with PolyangiitisWhile some symptoms of Granulomatosis with Polyangiitis — such as fatigue, a runny nose, or cough — may be misattributed to exhaustion or mild illnesses, other symptoms like repeated nosebleeds, chest pain, or shortness of breath are always a reason to vist your health care provider.
As with diagnosing any other medical condition, doctors follow a strict path of tests and exams when diagnosing Granulomatosis with Polyangiitis. First of all, they take the patient's history and go into details about every single symptom patients are suffering from. Then they perform a physical exam as well as ear, nose and throat examination (particularly if there is a history of nosebleeds and nose discharge), trying to reveal any structural or functional abnormalities.
What follows is blood testing. A complete blood count usually points to the presence of anemia (low red blood cell count) along with an increased erythrocyte sedimentation rate. One of the most significant blood tests performed in people who are assumed to be suffering from Granulomatosis with Polyangiitis is the one that detects autoantibodies, the aforementioned ANCA in particular. Approximately 90 to 95 percent of all patients have these autoantiboides circulating in their blood. However, the very presence of ANCAs in the blood is not sufficient for the diagnosis to be finally confirmed. This is because such antibodies are also detected in other autoimmune disease such as lupus erythematosus.
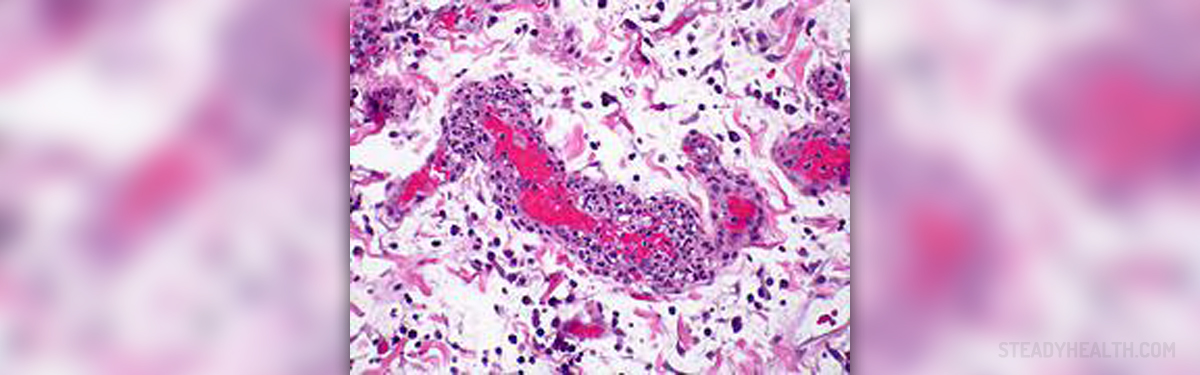
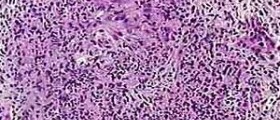
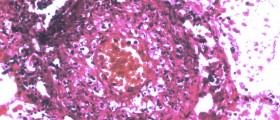
So, there is a need for further tests and exams. One of these, which is considered to be accurate enough for the confirmation of the condition, is a biopsy of the affected tissue. Under controlled circumstances, doctors take a sample of the tissue that shows signs of inflammation. The samples are inspected under a microscope. In the case of Granulomatosis with Polyangiitis, inflammation is in the specific form with specific cells forming specific structures (e.g. vasculitits and granulomas). This is of vital importance when differentiating the condition from other inflammatory illnesses.
And finally, it is essential to perform urine tests and evaluate the function of the kidneys because these organs are one of the targets of the inflammatory process. Additionally, chest X-ray reveals to what extent the lungs are affected and damaged.
All in all, Granulomatosis with Polyangiitis is a serious, potentially lethal, and hard-to-treat condition. If affects many organs and their blood vessels precipitating damage mediated by specific autoantibodies called ANCA. However, with timely treatment the progression of the disease can be at least delayed and current symptoms brought under control, and many patients achieve remission.
A note about the name Wegener's granulomatosisGranulomatosis with Polyangiitis used to be called Wegener’s Granulomatosis, and may still sometimes be referred to as Granulomatosis with Polyangitis (Wegener’s). A new name was selected for the condition in 2011 for several reasons:
Though the doctor Wegener the condition was named after in English was one of the earlier ones to describe the condition, he was not the first — and scientists have learned a lot more about the condition since it was first reported in the scientific literature. The new name reflects a greater understanding of the condition. The Dr Wegener after which Granulomatosis with Polyangitis was initially named was involved with the Nazi regime, something that further prompted modern scientists to make sure to change the name of the condition.We have updated this article accordingly.











-Symptoms,-Diagnosis,-Treatment_f_280x120.jpg)



Your thoughts on this
Loading...