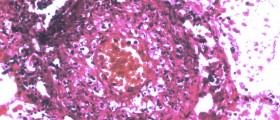
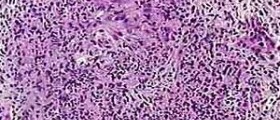
Urticarial vasculitis is a condition affecting the skin characterized by erythematous wheals that are quite similar to urticaria but there are specific changes that can be noticed at the microscopic level. Namely, histologically urticarial vasculitis occurs in the specific form of leukocytoclastic vasculitis.
What is Urticarial Vasculitis?
As a form of vasculitis, urticarial vasculitis may easily be further divided into normocomplementemic and hypocomplementemic. These subtypes apart from causing skin changes are also accompanied by systemic problems such as angioedema, pain in joints, abdominal/chest pain and increased body temperature. It is also possible for one to additionally develop pulmonary or kidney disease, inflammation of the uvea and Raynaud phenomenon. In the majority of cases systemic disease affects people suffering from hypocomplementemic urticarial vasculitis. This variant is also connected with systemic lupus erythematosus, a severe autoimmune disease.
When it comes to pathophysiology of the disease this type of vasculitis is relatively similar to other types of vasculitis that are in the nature leukocytoclastic and affect small blood vessels. The disease belongs to a group of type III hypersensitivity reaction. The inflammation is initially triggered by accumulation of antigen-antibody complexes inside the walls of the affected blood vessels. The build-up per se precipitates complement activation and chemotaxis of neutrophils. These cells are actually a type of white blood cells and contain many different proteolytic enzymes which, once released, may easily damage the wall of the affected blood vessels. Additionally, medical experts believe that in early stages of inflammation the body also sends eosinophils at the site of inflammation.
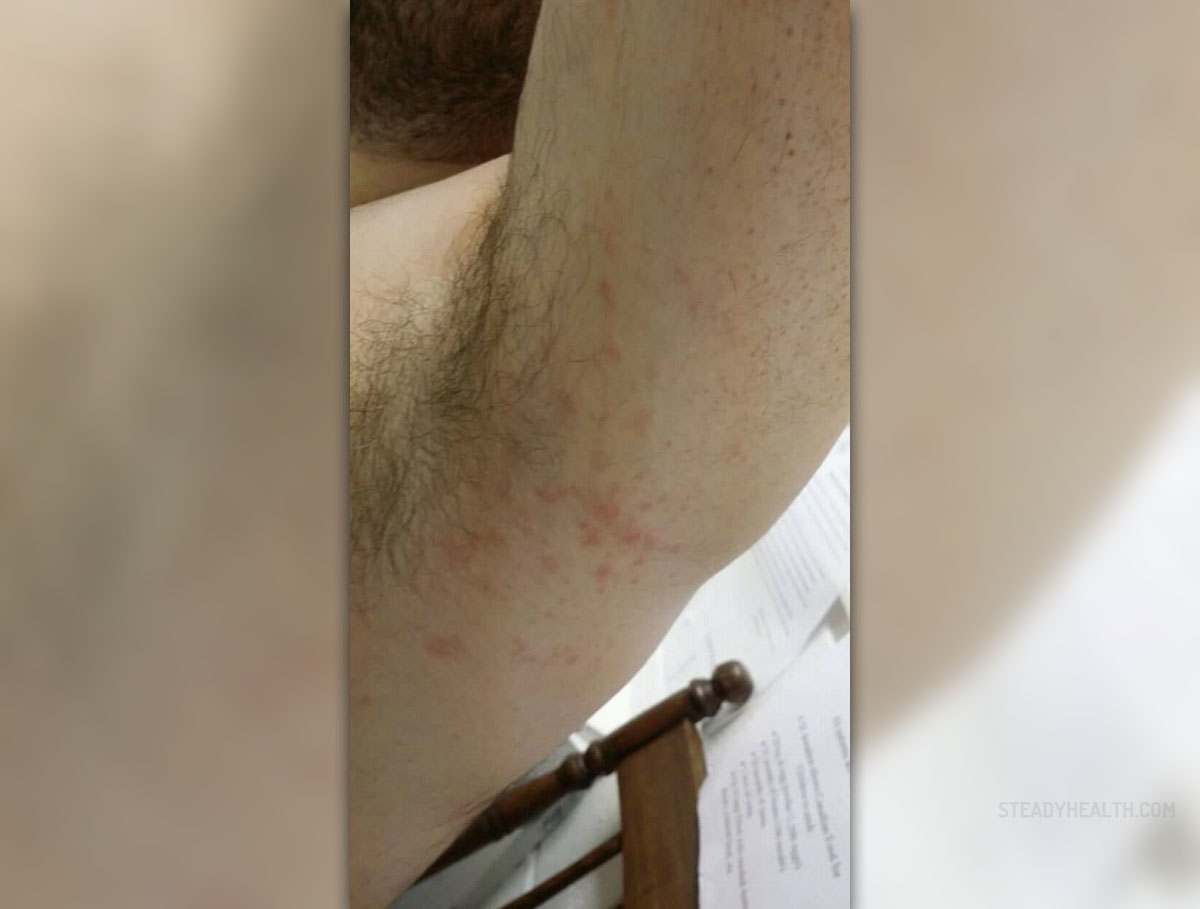
As far as symptoms and signs of urticarial vasculitis are concerned, these typically develop in the form of an urticarial eruption. The skin changes are very painful and may trigger burning sensation. The condition is generalized and there are erythematous plaques which tend to linger for 24 hours, disappear and new skin changes are formed. The changes, therefore, migrate but they do not resolve on their own. Some skin changes may additionally contain petechiae inside. Hyperpigmentation is sometimes seen once skin lesions withdraw. Fever, photosensitivity, enlarged lymph nodes, pain in joints and angioedema are several more issues these patients experience together with vasculitis. Abdominal/chest pain along with pericardial and pleural effusion may occur as well.
Even though scientist seem to be clueless regarding urticarial vasculitis there seem to be factors which contribute to the onset of this specific inflammation. Namely, many times the disease is associated with intake of certain drugs such as ACE inhibitors, penicillin, sulfonamides, NSAIDs etc. Furthermore, there is close connection between urticarial vasculitis and some autoimmune diseases. For instance, the condition can be associated with systemic lupus erythematosus and Sjögren syndrome. And finally, there is possibility that some viruses may precipitate inflammation of blood vessels in the skin. These include hepatitis B and C viruses and Epstein Barr virus.
What are Treatment Methods for Urticarial Vasculitis?
As it is the case with any other medical condition even in people suffering from urticarial vascular there needs to be gradual diagnosis and only once the condition is definitely confirmed one may start with best possible treatment.
Doctors first take patient's medical history and thoroughly examine the skin. Complete physical examination is of utmost importance because it may reveal lymph node enlargement and fever apart from typical skin changes. Along with blood tests and several more less invasive exams, in order to definitely confirm the condition doctors must take samples of the skin. Biopsy is performed and after pathohistological examination doctors can say for sure whether the inflammation is urticarial vasculitis or some other similar medical condition. Once the disease is confirmed it is essential to identify any potential associated disease patients may be suffering from. For example, laboratory studies may reveal changes in renal function. One may also have alternated immune status. What is more, some patients may be affected by pleural or pericardial effusion, both of which are considered serious health issues.
Urticarial vasculitis is a chronic condition with low mortality if there are no damage to vital organs such as the kidneys or the lungs. This is the reason why treatment must provide with long-term control over the process of inflammation. Drugs that are administered may precipitate toxic effects and because of that treatment must be carefully planned and doses precisely calculated.
Patients diagnosed with normocomplementemic urticarial vasculitis generally develop milder form of the disease and in them there is a chance for the skin changes to withdraw spontaneously. Others with more complex form of the disease and systemic manifestations require several different drugs. Inflammation is easily brought under control with non-steroidal anti-inflammatory drugs. Severe cases require long-term control over inflammation and potential damage to various internal organs. Most patients respond well to several drugs including Dapsone, colchicine, hydroxychloroquine, indometacin and corticosteroids. However, if these fail to provide with desirable results, patients receive more aggressive immunosuppressive therapy which includes azathioprine, cyclophosphamide and Cyclosporine.















Your thoughts on this
Loading...