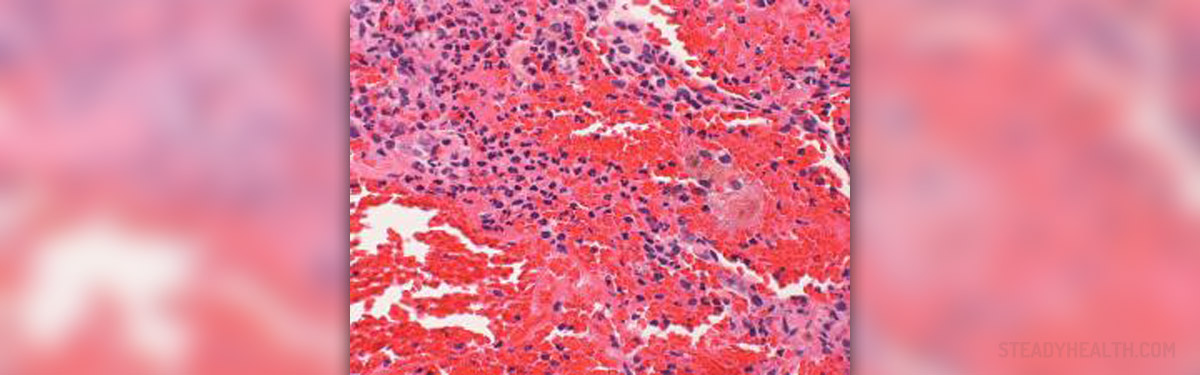
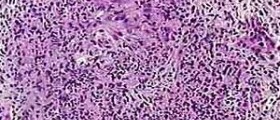
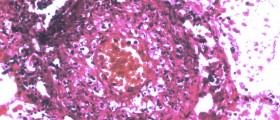
Wegener's granulomatosis (now known as granulomatosis with polyangiitis) is a rare disorder of the blood vessels. It is an inflammation of the blood vessels which affects the blood supply to other organs. Besides the inflammation, granulomas are formed around the blood vessels. Granulomas are a sort of inflamed tissue that damages healthy tissue.
Since Granulomatosis with polyangiitis can affect different organs, the symptoms of Wegener's can vary. Granulomatosis with polyangiitis can affect kidneys, lungs, skin, gastrointestinal tract, nervous system, and brain.
The signs and symptoms involve a runny nose, bleedings from the nose, pain in the sinuses, infection of the ear, coughing (sometimes coughing up blood), short breath, vision disturbances, pain in the eye, red eyes, pain in the joints, swelling of the joints, sores on the skin, loss of appetite, fever, and fatigue.
- The peak incidence is observed at 64–75 years of age, with a prevalence of 8–10 per million depending on geographic location.
- Although GPA was first described by Klinger as a form of polyarteritis nodosa (PAN), the unique nature of the disease was recognized earlier by Wegener. The term GPA was first introduced into the English literature in 1954 by Godman and Churg. This term, as opposed to Wegener's granulomatosis, describes the main pathologic feature (granulomatous inflammation) and reflects the vasculitic involvement of multiple types of vessels (polyangiitis).
- The incidence of GPA is estimated to be 8–10 cases per one million depending on geographic location. It has been suggested that the incidence of GPA is increasing, however this may simply reflect the availability of new diagnostic modalities and serologic tests such as anti-neutrophil cytoplasmic antibodies (ANCAs) that allows a more frequent diagnosis. The age of symptoms onset has a wide distribution with a peak incidence at 64–75 years of age.
- Previous studies showed that GPA can occur in children with 8–15% of cases occurring in patients age 19 or younger. Although slight male predominance has been reported in few case series, a recent study including 158 patients showed no sex predilection. GPA is most frequently reported in white Caucasian patients but can be seen in all racial and ethnic groups.
- In a survey of 701 North American patients with GPA, 30% of patients were reported to have ocular involvement. Other studies have reported similar findings, with ocular involvement in about 50% of the patients. Ocular disease can be the presenting or even the only clinically apparent manifestation of GPA.
- The average life expectancy for a patient with GPA without treatment is only 5 months, with a 1-year survival rate of less than 20%. It is a common misconception that the presence of an ocular manifestation in the absence of systemic manifestations represents a quiet disease. It should be noticed that ocular manifestations, particularly necrotizing scleritis, can be an indicator for both morbidity and mortality unless appropriate systemic treatment is initiated.
- Although the prognosis of GPA has dramatically improved with the introduction of immunotherapy, there is still significant morbidity from the disease itself (86%) or side effects from the therapy (42%). It has been shown that the presence of prior relapses is a predictor of future relapses.
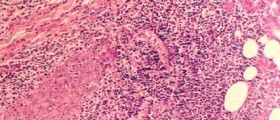
Diagnosis
In order to diagnose Granulomatosis with polyangiitis your doctor will order a special blood test which will reveal the presence of the disorder. To check if Granulomatosis with polyangiitis has affected the kidneys, a urine test will also be performed.
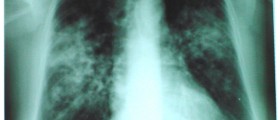
Additional tests will be done if there is a suspicion that Granulomatosis with polyangiitis affected some other organs. Such tests are X-ray images or CT scans of the lungs, bone marrow aspiration, and biopsy of the affected organ. The tissue for biopsy may be taken from the lungs, kidneys, nose, or skin.
Treatment
If Granulomatosis with polyangiitis was diagnosed on time and if you received the proper treatment, you can get better after several months. In addition, your condition must be monitored even after the recovery because the disorder may recur.
The treatment usually begins with corticosteroids which are enough for some patients. On the other hand, some patients may need additional medications to strengthen their immune systems. In case Granulomatosis with polyangiitis damaged your kidneys, you may need a transplant to regain the normal function of the kidneys.
Complications
Depending on the severity of the symptoms and the fact which organs are affected, Granulomatosis with polyangiitis can have some serious complications.
If the ear was involved, it may cause complete loss of hearing. If you developed skin sores as a consequence of Granulomatosis with polyangiitis, they may leave severe scars. Heart attack is also possible if arteries that are affected.
One of the most dangerous complications of Granulomatosis with polyangiitis is kidney failure. It may cause kidneys to retain fluid and waste inside them, and if the waste gets to your bloodstream, it can be a life-threatening disorder.
Other complications can include nose perforation, swelling of the eye, and lung failure. Some patients can have side effects from the medications.












Your thoughts on this
Loading...