Condyloma or genital warts are very widespread viral disease. It is believed that the infection affects one in three to four persons in the world. Genital warts are bulges formed by infected cells of the skin or mucous membrane, which usually occur in the genital and anal areas.
Causes
Condyloma is caused by human papillomavirus (HPV). So far, 80 types of the virus have been isolated, and it is considered that there are more than 100. Genital warts are not caused by all types of HPV virus. Some types of HPV cause warts on the hands and soles of feet, flat warts on the skin, mouth, and vocal cords.
Less risky types of HPV cause the appearance of condyloma in the genital area. Riskier types of this virus cause dangerous changes in the cervical mucosa (dysplasia) not causing any symptoms. Infection with HPV increases the risk of cervical cancer, which is more about the riskier types.

Fortunately, most women with positive HPV tests do not get condyloma, dysplasia, and cancer. The virus that causes condyloma does not cause cancer, but condyloma left untreated increases the risk of cervical cancer.
Transmission
Condyloma is a sexually transmitted disease. Viruses can enter the body if skin or mucous membranes are damaged and if there is direct contact with the skin or mucous membranes of an infected person or its secretions. Using a condom reduces the risk of infection, but the risk is not excluded, because genital warts are located on the areas that aren't covered with a condom.
Appearance and Location
Female condyloma usually appears on the back wall of the entrance to the vagina, small and large lips, perineum, rarely in the vagina, and cervix. In men, genital warts affect the prepuce (foreskin) alcove around the head and urethra opening. Less frequently, they occur on the scrotum and around the anus (except for homosexuals). Rarely, condyloma occurs on the groins and in the oral cavity.
Genital warts are usually soft elongated tubers of skin or mucosa that look like a cauliflower. They are whitish or pink. At first, they are small, but they can significantly grow to be numerous and form large panels.
Symptoms
Condyloma usually does not cause any discomfort - no pain, burning, or itching. Also, genital warts are often not noticed. Sometimes, it happens that the wart's surface is damaged causing infections. In this case, bleeding and a specific odor may occur.
Diagnosis
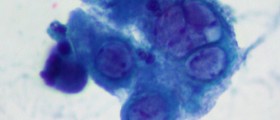
For the diagnosis gynecological examination, colposcopy, review under magnification, exfoliative cytology, biopsy, and determination of virus type in tissues and bodily secretions are used.
Treatment
Treatment of condyloma may be long-term. The most effective is the treatment of both partners, using condoms for several months after healing. Condyloma may be physically destroyed by Cryotherapy (freezing), thermal coagulation, Electrocoagulation, radio-coagulation, laser-vaporization, or surgical cutting. The least effective is freeze therapy, and the most effective is surgical removal.
Also, in the therapy anti-tumor drugs in the form of creams or ointments are used. Local interferon therapy gives poor results. The greatest success in treatment is achieved by a combination of laser therapy with cytostatics or laser plus interferon.
- Diagnosis by biopsy and viral typing is not recommended for routine or typical lesions.
- When podophyllin resin is used to treat genital warts, the skin should be washed one to four hours after application to reduce local irritation.
- Colposcopy, acetowhite staining, and other methods should not be used to.screen for subclinical warts in a general patient population or in patients with a history of genital warts.
- The choice of treatment depends on the number, size, and location of lesions; there is little evidence that any approach is more effective than another, although costs differ.
- Patients should be offered a follow-up evaluation two to three months after treatment.
Complications
Regardless of the method used in the treatment of condyloma, complications may occur. After the intervention, a person can experience burning during urination, pain when sitting, and enhanced and altered vaginal discharge. Rarely, pain and swelling in groins and a fever can also be present. In the first two to three months after the intervention, one may feel a sense of dryness, pain, or shooting of the lining or the outside of the genitals during sexual intercourse.















Your thoughts on this
Loading...