How is Bowel Surgery Performed?
Bowel operation may be performed two ways. The first involves making a wide cut along the area and performing open surgery. The second requires several small incisions to be made along the abdominal area and, by using special instruments the operation is performed through those incisions only.
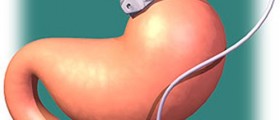
Bowel operation, in most cases, involves the removal of a part of the colon which is damaged by cancer or a similar disease. After removal, surgeons make sure that cancer has not spread any further and connect the remaining parts of the colon by using stitches or other procedures. However, sometimes, due to various causes, the colon cannot be reattached. Then as a permanent or a part-time solution a bag is connected to the end of the bowel and all the waste is expelled there. The bag is later emptied and a new one is applied.

Bowel Surgery Post-Op
After the operation, hospitalized recovery takes place. All the medications are applied intravenously and the patient is applied various compressors and bandages to keep the blood circulation high since it decreases the danger of complications appearing.
After a certain period of time, when the patient has recovered enough to feed on his or her own, he or she needs to intake moderate amounts of fluid while still having a catheter attached to collect the expelled urine.
While in home treatment, the patient should avoid straining during a bowel movement to prevent any damage to the reconnected colon. Pain control is crucial since pain can cause bowel contractions and may provoke damage. The recovery period lasts for about 12 weeks during which keeping in touch with the doctor is a must.
Possible Complications
Unfortunately, as with any surgical procedure, there are numerous complications that can take place during the recovery period. Pain and scar from the incisions made are the first. There is the danger of internal bleeding, various infections affecting the bowels, or spreading to other organs. The reattached colon may get disconnected damaging the internal organs, possibly leading to death. Nerve damage may occur if nerves were damaged during the surgery. This may be curable but may also cause permanent damage to the patient's bladder or sex organs.
- Multiple studies have evaluated predictors of overall morbidity following colorectal surgery. Patient factors predicting postoperative complications include older age, comorbidity (specifically neurologic or cardiorespiratory comorbidity), and low preoperative albumin. Operative variables found to predict morbidity included emergent operation, longer operative time (> 120 minutes), and peritoneal contamination.
- Both length of stay and postoperative readmissions have been used as markers of quality of care in recent years and preventable readmissions are increasingly tied to reimbursement. In colorectal surgery patients, distal anastomosis, benign pathology, open technique, older age, comorbidity, social deprivation, and low provider volume have been found to be risk factors for prolonged length of stay.
- In colorectal surgery patients, the development of multiple complications has been found be associated with worse postoperative outcomes including prolonged length of hospital stay (risk ratio [RR]: 2.8, 95% confidence interval [CI]: 2.3–3.2) and postoperative mortality (RR: 7.2, 95% CI: 5.1–9.7).
- Anastomotic leak following colorectal anastomosis is a relatively common complication and researchers have evaluated the relationship between leak and oncologic outcomes. A study of 1,181 rectal cancer patients demonstrated no relationship between anastomotic leak and local recurrence (p?=?0.669), overall recurrence (p?=?0.606), overall survival (p?=?0.648), or cancer related survival (p?=?0.421).
- As readmission following colorectal surgery is relatively common, identifying risk factors for readmissions and developing programs to prevent postoperative readmissions has been a popular area of research and quality improvement work. Not surprisingly, postoperative complications are a common cause for readmission in this patient population, and therefore, early identification and treatment of these complications as an outpatient are key to preventing readmission in these patients.
- An analysis of patients who underwent colectomy for colon cancer in the SEER Medicare database demonstrated an 11% readmission rate within 30 days.
- A study of colorectal patients who had complications requiring surgical intervention found that patients with complications were less satisfied with their physicians. Patients judged their satisfaction with the quality of care and the following physician areas: interpersonal skills, technical skills, information provision, and availability to be worse than in patients without such complications. The presence of postoperative anastomotic leak was an independent predictor of quality of life.
If the procedure involves making smaller incisions as mentioned at the very beginning of this article, it may go unexpectedly wrong and open surgery may be necessary.
Many things may go wrong, but many things are wrong as long as the surgery is a must in the first place. Although there are many risks mentioned here, these are mere possibilities and most of the times the side effects of bowel surgeries are minor and easily treatable.
- www.nhs.uk/conditions/bowel-cancer/treatment/
- www.nhs.uk/conditions/colostomy/risks/
- Photo courtesy of Olga Guryanova by Unsplash: unsplash.com/photos/tMFeatBSS4s














Your thoughts on this
Loading...