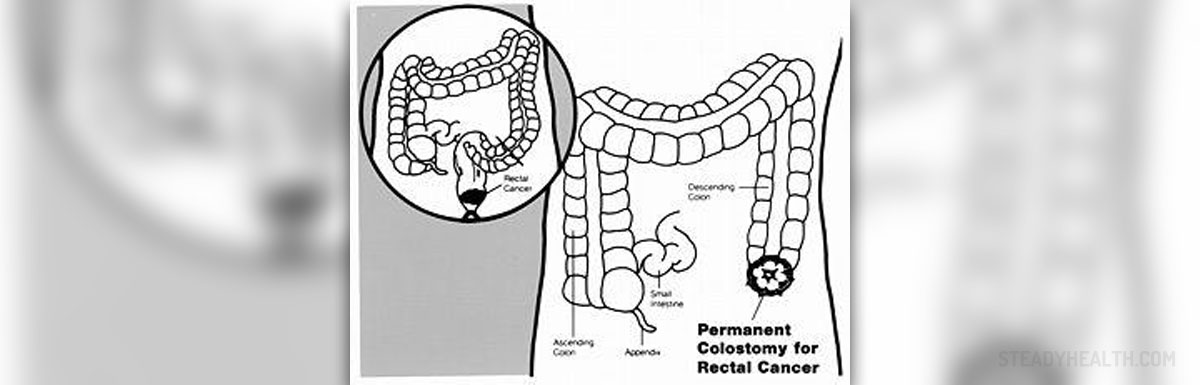
A colostomy is a surgical procedure in which an opening called stoma is created in the anterior abdominal wall to bring out the healthy end of the large intestine and suture it into the abdominal opening. This operation is done to provide an alternative channel for feces to leave the body. A colostomy is indicated in many conditions such as colon cancer, diverticulitis or abdominal injury. However, this procedure can be reversed in a procedure known as colostomy reversal surgery.
Colostomy Reversal Surgery Overview
Colostomy reversal surgery is a surgical procedure done to restore the function of the intestine and the rectum. This operation is usually performed as an open surgery but sometimes it may be done as laparoscopic reversal surgery, which is a minimally invasive procedure. The type of colostomy reversal surgery is not determined by the type of the prior colostomy surgery.
The patient is admitted to the hospital a few days before the surgery. To prepare for the procedure, the patient is given a medicine that helps to flush out bowels. Colostomy reversal surgery is done under general anesthesia.
In laparoscopic colostomy reversal surgery, a surgeon makes two incisions below the navel. These incisions enable the surgeon to insert surgical equipment and a laparoscope. Then the abdominal wall of the patient is lifted and detached from the internal organs by filling of the abdominal cavity with carbon dioxide. The rectum and the colon are reconnected with the help of a stapling device. Finally, the incisions are stitched close.
Recovery time for colostomy reversal is between six to ten days. The patient is advised to be physically active to speed up the recovery. Being physically fit before the procedure also makes the recovery quicker.
Side Effects of Colostomy Reversal Surgery
The main side effect of colostomy reversal procedure lies in a length of time required for the bowel to begin functioning again. This may take a few days or much longer because the rectum was not used while there was an anterior stoma in the body.
Since a colostomy causes muscles of the intestine to weaken, the patient may experience interrupted or irregular bowel movements after colostomy reversal surgery. Diarrhea or constipation may develop as a side effect of the procedure.
The patient may experience bleeding during bowel movements or have bloody stools. Mild pain and tenderness in the abdomen may occur too. Less frequent urination and inability to drink or eat are other potential side effect of colostomy reversal.
Finally, as with any operation, the patient may have allergic reaction to anesthesia or the wound may get infected.
- During the study period 170 patients underwent defunctioning ileostomy following anterior resection for sigmoid or rectal cancer. The median age (range) was 69 years (41 - 90 years). Of these patients, 117/170 (68.8%) were male.
- Of the 170 patients who had defunctioning ileostomies, 127 (75%) underwent subsequent reversal of ileostomy. Median time to reversal was 6 months (range: 1 - 42 months). Of these ileostomy reversals, 63/127 (50%) were delayed longer than 6 months. The reasons for delay were due to adjuvant chemotherapy in 22/63 (35%), surgical complications in 13/63 (21%) which included anastomotic leak following the initial operation in 9/63 (14%), adhesive small bowel obstruction in 3/63 (5%), and anastomotic stricture in 1/63 (2%) patient. Medical complications were seen in 14/63 (22%), which included eight patients with acute kidney injury due to high output stoma.
- The median length of inpatient hospital stay following reversal of ileostomy was 4 days (range: 1 - 62 days). Postoperative complications occurred in 33/127 (26%) patients. There was a statistically significant rate of complications following reversal and a median length of hospital stay following reversal of > 4 days in the delayed group. A further 5/127 (3.9%) patients were re-admitted within 30 days for postoperative complications. There was no postoperative mortality.
- The following causes were associated with having a permanent stoma: cancer stage IV 23% (10/43), patient refusal 14% (6/43), patient death prior to reversal 11% (5/43) and other causes 21% (9/43), pelvic recurrence, high risk, refashioning of ileostomy, rectovaginal fistula, and medical illness.
- The major finding in this study was that reversal of ileostomy in patients having delayed closure is associated with increased risk of complications and increased length of hospital stay. Of those that are closed, approximately 50% have delayed closure > 6 months following their ileostomy formation. Also, one in four defunctioning ileostomies are not closed following anterior resection for rectal cancer in our unit. In 50% of the patients, the delay could be explained by postoperative adjuvant chemotherapy, non-surgical complication and symptomatic anastomotic leakage and small bowel obstruction.














Your thoughts on this
Loading...