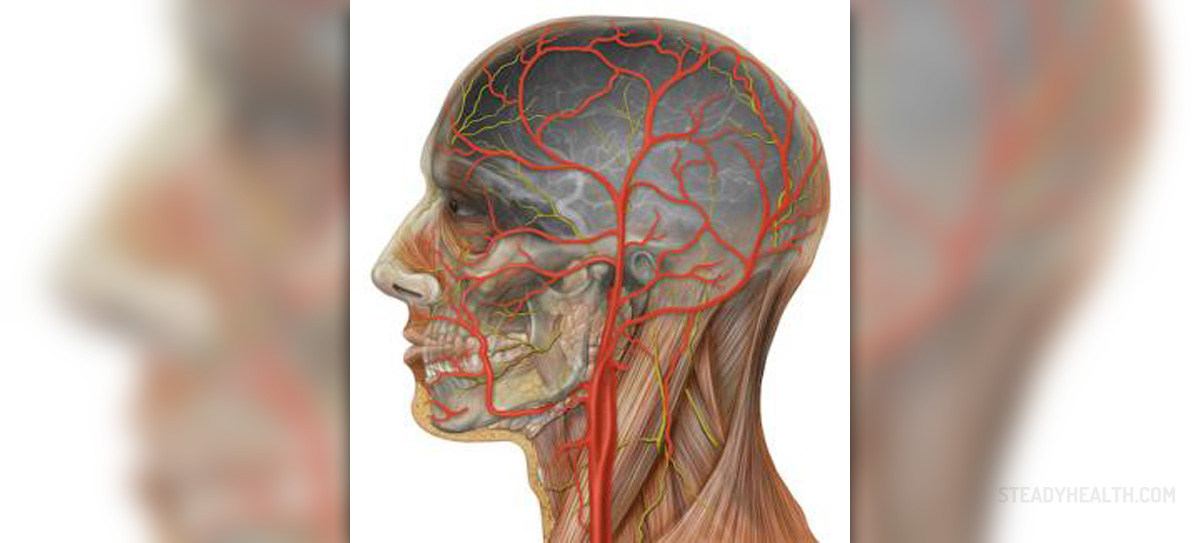
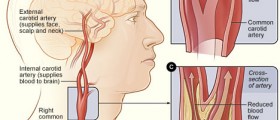
The carotid artery is a blood vessel located on each side of the neck. It carries blood to the brain and also supplies the structures of the face. Narrowing of the carotid artery generally occurs due to atherosclerosis, and its blockage can result from an additional build-up of blood clots.
The most common symptoms and signs of carotid artery blockage include dizziness, fainting, severe headache, blurred vision/ loss of vision, and confusion. A patient may also experience a mild stroke and have speaking and swallowing difficulties.
Carotid artery surgery is a surgical procedure performed to restore the flow of blood rich in oxygen and glucose to the brain in patients suffering from carotid artery blockage.
Carotid Artery Blockage - Treatment Options
Carotid artery blockage can be successfully treated with endarterectomy and angioplasty (with stent placement).
Carotid artery blockage surgery or endarterectomy is performed under general or local anesthesia. The surgeon reaches the affected artery with a cut on the neck exactly over the carotid artery. Until the affected part of the artery is cleaned a flexible tube is placed in the place of the carotid artery, and it transfers the blood during surgery. The affected part of the carotid artery is treated with plaque removal, and the artery is closed with stitches. It is essential to monitor heart and brain activity during the entire procedure.
- Current clinical guidelines for both primary and secondary prevention of stroke in patients with carotid stenosis caused by atherosclerotic plaques remain reliant on general patient characteristics (traditional risk factors; hypertension, smoking, diabetes, and hypercholesterolemia) and static measures of the degree of artery stenosis.
- Atherosclerotic lesions develop slowly over many years, passing through several stages. Risk factors for atherosclerosis such as hypertension, diabetes, smoking, hypercholesterolemia, genetic disposition, infection, and elevated homocysteine can activate pro-inflammatory and anti-thrombotic responses that induce endothelial dysfunction.
- In the event of plaque rupture, the plaque content including the thrombogenic lipid core is exposed to blood containing platelets and coagulation factors with a resultant high risk of thrombus formation. Cerebrovascular symptoms are the result of these thrombi causing vessel occlusion at the plaque location and/or emboli that are carried in the blood stream to the brain where they occlude cerebral blood vessels.
- Traditionally, atherosclerosis has been viewed as a slowly progressive, cholesterol storage disease involving the passive accumulation of cholesterol debris in the arterial wall. However, atherosclerosis is now accepted as a generalized inflammatory disease. In fact, inflammation plays an important pathogenic role in all stages of atherosclerosis including the destabilization of atherosclerotic plaques.
- In addition to CRP many different inflammatory mediators involved in the atherosclerotic process have been measured in plasma and found to be associated with plaque instability (fibrinogen, leukocytes MMP-7, IL23, visfatin granzyme B CD-36 IL-6 VCAM-1). However, thus far no single biomarker has been found able to reliably predict ischemic stroke or CVD.
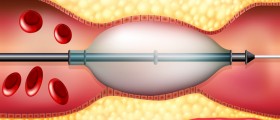
Carotid angioplasty and stenting are not invasive as carotid artery blockage surgery. In this case, the patients are administered relaxants and numbing medications. The surgeon cuts the groin area and inserts a catheter into an artery. The catheter is led to the neck with the assistance of a specific X-ray called a fluoroscope, and finally, once the blockage is identified, a guide wire is passed through the catheter. The guide wire is essential for passing over a catheter with a tiny balloon. The balloon is blown up and it mechanically removes the plaque. This way, the carotid artery restores its normal diameter.
In some people, a stent is inserted together with the balloon catheter and left in place of the blockage. The role of a stent is to expand when the balloon is blown up, and it additionally keeps the artery open. At the end of the procedure, the balloon is deflated and removed.
Risks of Carotid Artery Blockage Surgery
The most common risks associated with carotid artery blockage surgery include heart attack, brain damage, allergic reaction to the dye used during the procedure, and formation of blood clots or bleeding in the brain.
In rare cases, the patient may develop seizures and stroke after the surgery. The blockage may become even more severe after the surgery (which generally occurs after a certain period).














Your thoughts on this
Loading...