Angioplasty - Overview
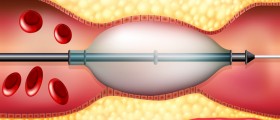
Angioplasty is a procedure that includes widening of narrowed or blocked blood vessels. The narrowing and blockage result from the process of atherosclerosis. The very procedure includes the insertion of an empty and collapsed balloon on a guide wire (balloon catheter) in the narrowed arteries.
Once the balloon catheter is inserted in the right location it is inflated to a certain size. The inflated balloon crushes the fatty deposits on the wall of the blood vessels and allows more blood to flow. Once the desired effect is achieved the balloon is collapsed and removed.
Angioplasty is usually performed in people suffering from diabetes, hypertension and high cholesterol levels, etc since these medical conditions carry a significant risk of atherosclerosis.
Angioplasty - Risks and Possible Complications
Even though angioplasty is considered a quite safe procedure it carries some risks. All the complications related to angioplasty can be divided into acute complications and long-term complications. Acute complications after angiography develop either during the procedure or immediately after while long-term complications usually develop several months after angioplasty.
Acute complications of angioplasty include abrupt closure of the treated artery during the procedure. This complication is considered very dangerous since it may induce a heart attack. Furthermore, a heart attack can also result from dislodging of a blood clot during the procedure. Dislodging of a blood clot may eventually result in complete blockage of the artery and cut off the inadequate oxygen supply. In case any of the previously mentioned complications occur the patient may require emergency bypass surgery.
Restenosis is considered a long-term complication of angiography. The very term refers to a repeated narrowing of the already treated blood vessel. Restenosis commonly occurs several months after the procedure. The problem can be caused by blood clots that develop at the very site of the treatment.
This can be prevented with Aspirin, heparin and other anti-clotting medications. These drugs are administered prior and after the procedure. Furthermore, coronary stents are also rather effective in the prevention of blood clot formation. Why restenosis actually occurs is now being investigated.
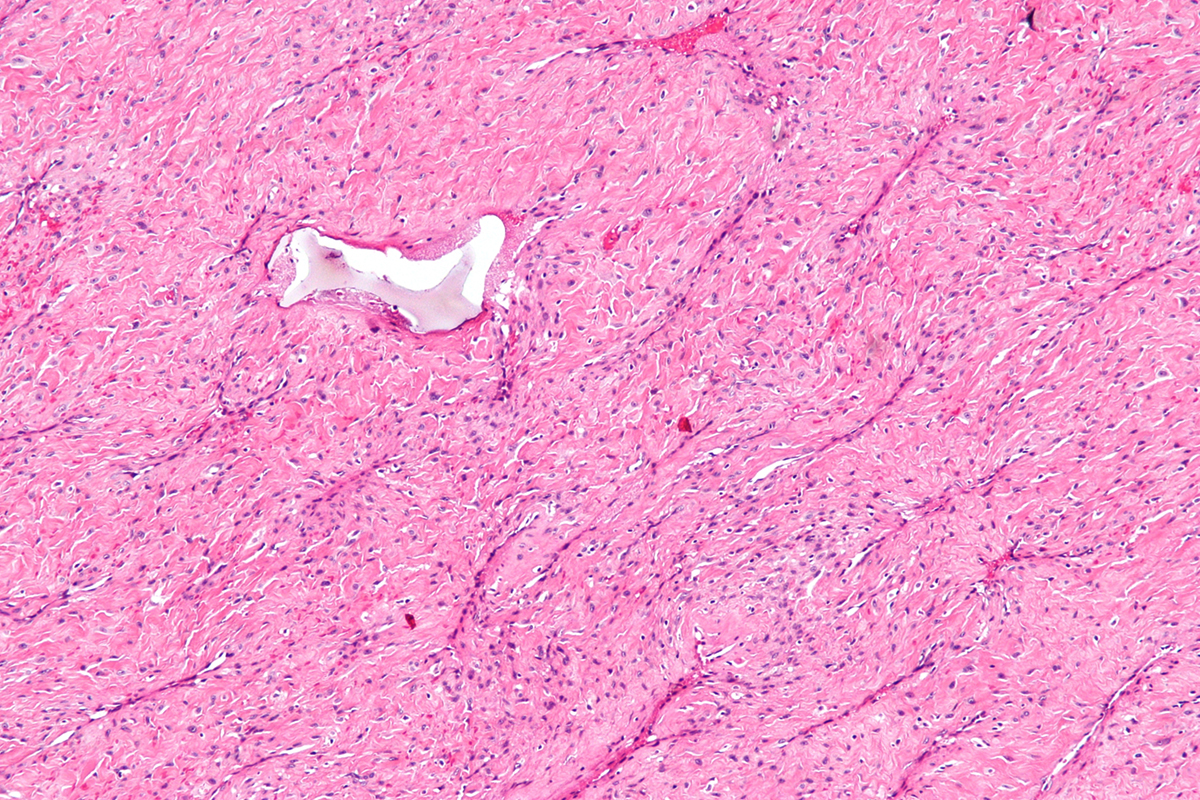
The scientists believe there are three complex mechanisms involved in the very process of restenosis. Namely, after the surgery (within hours) the walls of the artery may start to withdraw and eventually regain their initial size. This way the channel can shrink up to half of its obtained size. Additionally, by making tiny cracks in the plaque even the wall of the artery suffers a certain amount of injury.
This damage leads to a collection of blood cells involved in the process of clotting and they eventually cause restenosis of the treated artery. Restenosis usually affects people who already deal with certain medical conditions such as high blood pressure, diabetes, angina and kidney disease (treated with dialysis).
- One rare but serious complication of angioplasty is iatrogenic coronary artery perforation (CAP) due to underlying complex lesion, occurring in 0.1% to 0.8 % of total cases undergoing angioplasty. CAP can be due to angioplasty guide wire perforation, balloon oversizing, and use of atherectomy devices. Management of CAP depends on the severity of the lesion, hemodynamic status, and Ellis class type of CAP.
- Complication of CAP is ST-segment elevation myocardial infarction, and early or delayed cardiac tamponade with or without hemodynamically instability which can require emergent pericardiocentesis.
- In-stent restenosis (ISR) is defined as the reduction in vascular luminal diameter after percutaneous intervention (PCI). The underlying pathophysiology of ISR depends on the type of stent used during PCI. In case of plain old balloon angioplasty (POBA), it is acute in onset because of elastic recoil and vascular remodeling.
- Stent fracture (SF) is an infrequently reported adverse outcome of DES use during PCI which can either occur periprocedural or later on when drug elution has been completely done. SF has also been linked to the development of ISR and stent thrombosis. Irrespective of the type of intervention done during PCI, ISR can also be due to neoatherosclerosis.
- The incidence of ISR in the pre-stent era was 32% to 55% of all PCI done, 17% to 41% for BMS, and for second generation DES and DEB it dropped to less than 10% of total PCI done. Such a low rate is due to the evolution of stents under strong criticism and advanced technology.















Your thoughts on this
Loading...