What is Cardiac Catheterization and When is it Done?
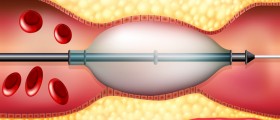
Cardiac catheterization is a procedure that consists of inserting a long catheter in a vein or artery either in an arm, leg, neck, or in groin and from there the catheter is lead to the heart all the way through the blood vessels. The procedure can be used for two reasons, in the treatment of various heart conditions, such as angioplasty, for example, or in order to check the condition of cardiovascular system and test for a heart disease.
In the first case, there are three procedures that cardiac catheterization is a part of, and these are: angioplasty, which may also include stent placement (though not necessarily) and which helps in expending and widening the blocked artery; closure of holes in the heart which are congenital; and balloon valvuloplasty, when narrowed heart valves have to be open.

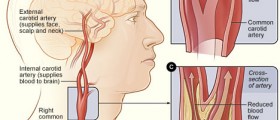
In the second case, when heart and other parts of cardiovascular system have to be checked, this procedure is used in the following situations: when the blockage or narrowing in blood vessels has to be located, when the amount of oxygen and/or pressure in the heart has to be determined, when congenital heart defects have to be diagnosed, or when a tissue sample has to be taken from the heart for the purpose of biopsy.
Whichever the reason, the patient will need several hours to recover from the procedure and from the anesthesia, and he will spend them in the recovery room and a regular hospital room. The part of the body used for the procedure should not be moved, so that the bleeding would be avoided. Some patients may go home the same day, while others are required to stay for a few days, but it depends on their condition.
Complications of Cardiac Catheterization
Having in mind that this procedure involves heart and blood vessels, there certainly have to be some risks involved, and some complications are possible. However, none of the major complications is frequent. Bleeding,infection and bruising of the surgery site are possible complications of every procedure,and so of this one as well.
Complications which are typically possible during or after cardiac catheterization are stroke, heart attack, arrhythmia or irregular heart rhythms, allergic reactions. It is also possible that the artery or vein, through which the catheter was inserted, is damaged, or that the tissue of the artery or heart is torn during this procedure, but it is important to mention that blood clots can also occur after the procedure. Kidney damage is one of the possible complications as well.
- There are no absolute definitive contraindications for cardiac catheterization procedures. Most of the contraindications are relative depending on the indication for the procedure and the associated comorbidities of the patient. When the risk of complications is expected to be more than what is considered acceptable for the procedure, alternative modes of imaging and assessment can be used to answer the clinical question.
- Most of the procedures can be performed with minimal or moderate sedation with the help of a local anesthetic, but some procedures will require anesthesia services for providing deep sedation or general anesthesia. Some of these procedures can be performed at the bedside in a coronary care unit, and the common ones performed bedside include right heart catheterization and temporary pacer wire insertion.
- The risk of major complications during diagnostic cardiac catheterization procedure is usually less than 1%, and the risk and the risk of mortality of 0.05% for diagnostic procedures. For any patient, the complication rate is dependent on multiple factors and is dependent on the demographics of the patient, vascular anatomy, co-morbid conditions, clinical presentation, the procedure being performed, and the experience of the operator. The complications can be minor as discomfort at the site of catheterization, to major ones like death.
- Hematomas are usually formed following poorly controlled hemostasis post sheath removal. Most hematomas are self-limiting and benign, but large, rapidly expanding hematomas can cause hemodynamic instability requiring resuscitation with fluids and blood.
- When the hematoma maintains continuity with the lumen of the artery, it results in the formation of a pulsatile mass locally, defined as a pseudoaneurysm. This will be associated with a bruit on examination.
- Direct communication between the arterial and venous puncture sites with ongoing bleeding from the arterial access site leads to the fistula formation and is associated with a thrill or continuous bruit on examination. These usually will require surgical exploration as they are unlikely to heal spontaneously and may expand with time.
- Dissection occurs in patients with an increased atherosclerotic burden, tortuous arteries, or traumatic sheath placement.
- Thrombosis and embolism are extremely rare with the use of low-profile catheters, and predisposing factors include small vessel lumen and associated peripheral arterial disease, diabetes mellitus, female sex, large-diameter sheath, and prolonged catheter dwell time.
- The most frequent complication after transradial access is about a 5% risk of radial artery occlusion. This is a clinically insignificant complication if the Allen test is normal. Patients with incomplete palmar arch and abnormal Allen test may have symptoms of hand ischemia after radial artery occlusion.













Your thoughts on this
Loading...