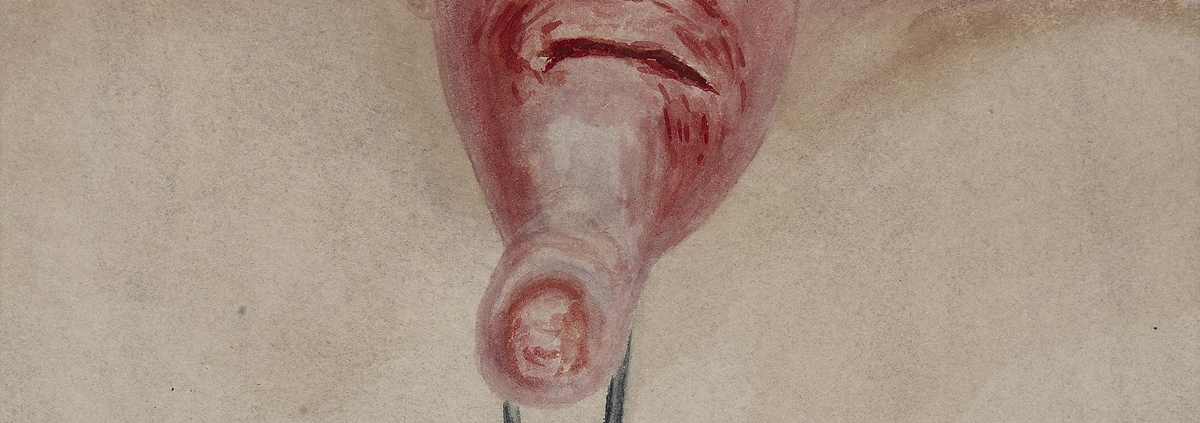
Rectal Prolapse Surgery Overview
Rectal prolapse surgery is a medical procedure that is done in order to repair the prolapse of the terminal part of the colon. Prolapse of the rectum can be partial or total and is rather embarrassing and problematic.
The surgery takes care of all the symptoms including problems with fecal incontinence. There are several surgical approaches in case of rectal prolapse. The surgeon makes the final decision which of the approaches is most suitable in a particular case. Basically, the operation is performed under general anesthesia and the patient needs to spend several days in hospital.
Risks of Rectal Prolapse Surgery
This surgery can result in some serious complications. They include bleeding, obstruction of large intestines, reversible or irreversible damage of the surrounding tissue or organs and infections. The condition may reoccur and some patients even complain about worsening of already present constipation. In rare cases, the rectum may become too narrow.
Rectal Prolapse Surgery Guide
The surgeon makes the final decision on how the patient will be operated on. This depends on the degree of the rectal prolapse, additional medical conditions and surgeon's experience. There are several types of surgery and they include repair of the rectum through the anus, repair through the abdomen and minimally invasive surgical approach.
In first approach the surgical procedure is performed through the anus. This procedure is also known as perineal rectosigmoidectomy. This procedure includes the removal of one part of the rectum while the remaining part is stitched to the colon. Even though this operation is done under general anesthesia for those patients who may have problems with general anesthesia perineal rectosigmoidectomy can be performed under regional anesthesia. The risk of complications is minimal.
The second option is repair through the abdomen or rectopexy. The surgeon places the prolapsed rectum back into the pelvis and attaches the rectum to the tissues that surround rectum and coat sacrum. This procedure carries more risk of potential complications comparing to the previous one.
And finally, the last option is minimally invasive surgery. It features with several small incisions on the abdomen. This is why this procedure is called laparoscopic rectal prolapse surgery. A camera together with certain instruments is used in this operation and the risk of potential complications is low.
- The most common coexisting anatomical abnormalities are a redundant sigmoid colon, diastasis of the levator ani, a deep cul-de-sac, a patulous anal sphincter, and the lack of rectal-sacral attachments.
- Women are more commonly affected; the female/male ratio is approximately 10:1. The incidence in the female population peaks in the seventh decade, with 50% of female patients being over the age of 70 years.
- Patients with rectal prolapse have various symptoms such as anal incontinence, constipation, mucus discharge, and hemorrhage. Approximately 50% to 75% of patients with rectal prolapse report fecal incontinence, and 25% to 50% of patients report constipation.
- Hemorrhage occurs frequently when the prolapsed rectum is left unrestored. Pelvic organ prolapse, including bladder prolapse, uterine prolapse, or rectocele, may also be combined.
- Recently, an abdominal approach via laparoscopy has emerged as an effective tool for the treatment of rectal prolapse. Previous studies have suggested that laparoscopic surgery has many short-term advantages over open surgery, including less pain and blood loss, shorter hospital stays, and faster recovery.
- A total of 4,175 patients were included in the review. Recurrence was reported to occur in 52/1,697 (3%) patients after the laparoscopic approach and 432/2,464 (18%) patients after the perineal approach. The recurrence rates after different laparoscopic procedures were 2% to 5%, and those after different perineal procedures were 16% to 20%. Laparoscopic procedures had a lower recurrence rate compared with perineal procedures.
- The mortality rate after each operative approach was similar (laparoscopic 0.5% vs. perineal 0.7%). There was no recorded mortality after laparoscopic suture rectopexy.
- The complication rate after laparoscopic procedures and perineal procedures was 12% and 14%, respectively. Forty-three studies that evaluated postoperative bowel symptoms reported an improvement of fecal incontinence in 71% of patients after laparoscopic procedures and 63% after perineal procedures. Improvement of constipation was reported in 57% after either laparoscopic or perineal approaches.
After the surgery the patient has to spend a few more days in the hospital and then he/ she is released. While in hospital until the proper function of rectum is re-established one is allowed to drink liquids and after a few days to consume solid food.
- www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/rectal-prolapse
- medlineplus.gov/ency/article/002932.htm
- Photo courtesy of St Bartholomew's Hospital Archives & Museum via Wikimedia Commons: commons.wikimedia.org/wiki/File:Prolapse_of_the_rectum_Wellcome_L0061308.jpg

















Your thoughts on this
Loading...