Brain hemorrhage is a serious medical condition accompanied by many complications and it may also be lethal. Since the brain is in charge with many functions in the body the symptoms and signs of the brain hemorrhage actually depend on the location of bleeding. Any bleeding into the brain is serious and requires prompt and suitable treatment.
Causes of Massive Brain Hemorrhage
Brain hemorrhage can occur due to several factors and illnesses. Brain injury is only one of them. Furthermore, brain aneurysm represents a condition in which certain arteries of the brain are dilated and may burst. Once they rupture (most commonly due to elevated blood pressure) bleeding starts and in some cases it may be very intensive and simply uncontrollable.
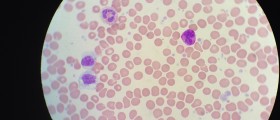
Rupture of the brain vessels is also possible if they have been affected by the process of atherosclerosis and their wall have weakened. Increase in blood pressure may cause burst of the structurally changed blood vessels. Amyloid angiopathy is another condition which carries a risk of brain hemorrhage. Bleeding from the brain blood vessels is also possible in patients suffering from certain structural abnormalities of blood vessels, hemophilia, sickle cell anemia and liver disorders.
Symptoms of Massive Brain Hemorrhage
The symptoms and signs of brain bleeding generally depend on the very location of bleeding and the amount of blood that has left the blood vessel. In massive brain hemorrhage the symptoms and signs are intensive and serious.
Patients commonly report sudden and severe headache, general body weakness or even paralysis of one side of the body, loss of balance and coordination and depletion of motor skills.
Seizures may be also a sign of massive brain hemorrhage. Huge loss of blood is typically accompanied by loss of consciousness and patients may even end up in a coma. Increased amount of blood inside the cranium leads to increase in intracranial pressure and subsequent nausea and vomiting.
Treatment for Massive Brain Hemorrhage
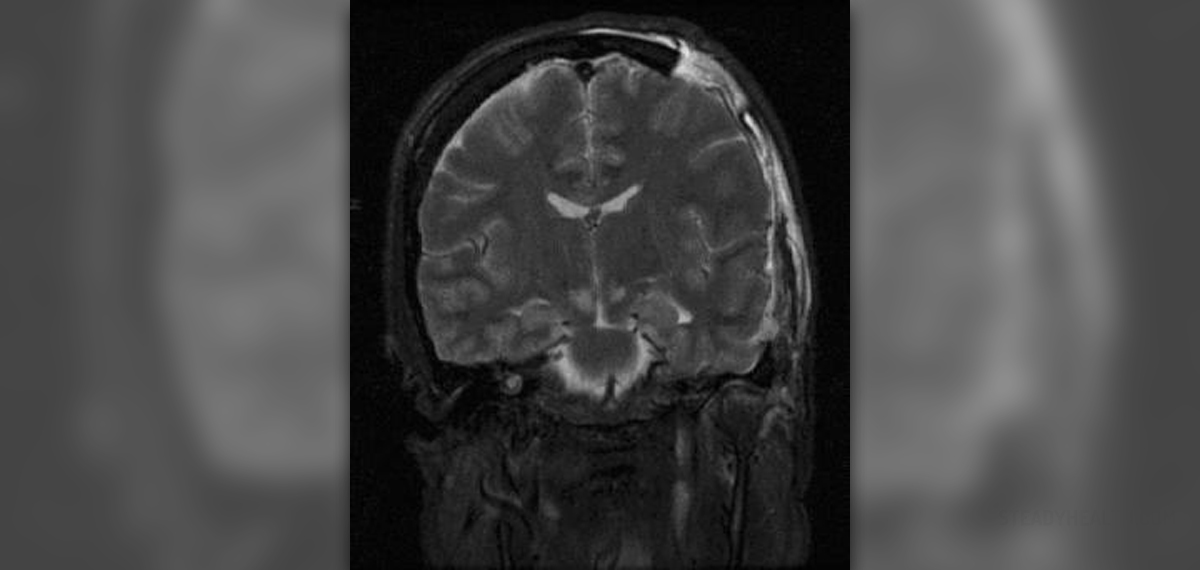
Massive brain hemorrhage is a serious condition and it requires prompt medical attention. Patients are always hospitalized and they undergo physical and neurological exam and conformation of the bleeding is achieved with the assistance of CT scan of the head. Lumbar puncture may show the presence of blood in cerebrospinal fluid and eye exam may point to swelling of the optic nerve.
Patients are treated conservatively and surgically. The most commonly prescribed medications include corticosteroids, diuretics and pain killers. Anticonvulsants are administered in case of seizures. Severe bleeding and subsequent swelling of the brain can be also treated surgically.
The outcome depends on the degree of damage to the brain cells. In many cases of massive brain hemorrhage patients end up with many neurological sequelae. Total paralysis and coma are common complications. And finally, there is also a chance of lethal outcome.
Massive Brain Hemorrhage and COVID-19
This article reports the clinical features of a COVID-19 patient whose first symptom was cerebral hemorrhage. More importantly, after the craniotomy, the patient had high fever and it was difficult to retreat. After cerebrospinal fluid testing, it was determined that an intracranial infection had occurred.
After anti-infection and plasma infusion of the recovered person, the patient’s symptoms gradually improved. This case suggests that COVID-19 may infringe on cerebral blood vessels and cause cerebral hemorrhage. Transfusion of plasma from rehabilitation patients is effective for critically ill patients.
- SARS-CoV-2 can invade the cardio-cerebrovascular system and damage the nervous system. Angiotensin converting enzyme 2 (ACE2) is highly expressed in human tissues such as the vascular endothelial cells, heart, liver, digestive tract, and kidneys. Studies have found that ACE2 is an important target for SARS-CoV-2 infection in humans. After infection, ACE2 levels are reduced or even absent.
- After SARS-CoV-2 infection, most patients were cured, but many patients progressed to severe illness and eventually died. Respiratory failure is the main cause of death, followed by sepsis (multiple organ failure), heart failure, bleeding, and kidney failure. The affected organs mainly include the respiratory system, cardiovascular system, coagulation function, and the liver and the kidney. In many cases, multiple organ functions are impaired.
- Through the study of death cases, it was found that in addition to directly attacking human tissues and organs, SARS-CoV-2 caused a cytokine storm by stimulating the human immune system. Many patients with severe COVID-19 will develop cytokine storm, which is an over-immune response of the human body. The main reason is the over-activation of non-specific immune cells, which release a large number of pro-inflammatory factors, such as interleukin-1, interleukin-6, and tumor necrosis factor.













Your thoughts on this
Loading...