Cerebral Hemorrhage – Causes, Symptoms, and Treatment
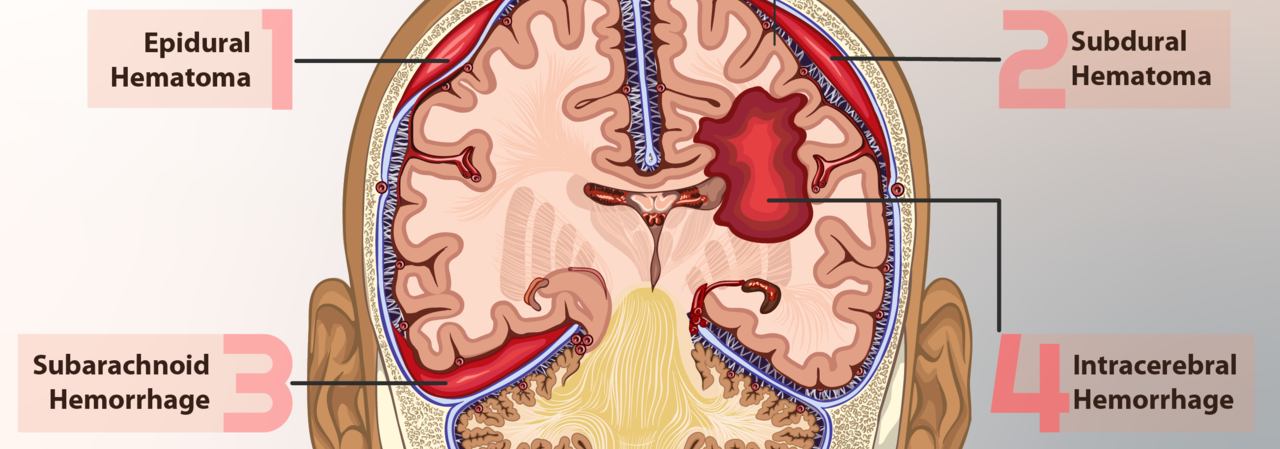
Cerebral hemorrhage or brain hemorrhage is the rupture of a blood vessel in the brain, which might cause brain bleeding and damage the central nervous system.
Brain hemorrhage is usually caused by head trauma, uncontrolled high blood pressure, abnormalities in the blood vessels, or amyloid angiopathy (abnormality of the blood vessels caused by aging that causes small unnoticed brain bleeding). Brain tumor or aneurysm may also be the cause of cerebral hemorrhage.
Some people are more prone to develop this medical condition than others. Risk factors for cerebral hemorrhage include people suffering from diabetes, hypertension, hemophilia, leukemia, sickle cell anemia, liver patients, smokers, alcoholics, and women in menopause. Unconsciousness, painful headaches, nausea, vomiting, weakness, paralysis, loss of vision, problems with speech, and sudden confusion all indicate that the patient might experience cerebral hemorrhage.
Treatment depends on the cause, location, and severity of bleeding. In any case, those patients need urgent medical attention. Doctors might prescribe anti-seizure medications, painkillers, diuretics, and corticosteroids. If the hematoma is larger than 3cm in diameter, a surgical procedure is the only option.
Cerebral Hemorrhage – Prognosis
Some patients might completely recover, some will have certain consequences and problems because of the hemorrhage, and others won’t survive the cerebral hemorrhage. The severity of the bleeding and the area of the brain that’s affected decide the patient’s prognosis.
Epidural hemorrhage is the bleeding between the skull and the brain covering. Even if a patient does get urgent medical attention, there are 15% chance that he/she would die. If the patient survives the epidural hemorrhage, it is most likely that he/she would never get the orientation back.
Intracerebral hemorrhage might be caused by brain injury, aneurism, or hypertension. The bleeding leads to brain swelling and produces heightened pressure in the brain. The prognosis for this condition is usually very good if the patient gets the proper medical care.
- We searched Ovid Medline 1946-2011 inclusive for cohort studies of ?50 patients reporting long-term (>30 days) outcome after ICH. Two reviewers independently extracted data from each study. We meta-analysed 1-year and 5-year survival data from population-based studies using a random effects model (and quantified inconsistency using the I2 statistic).
- We identified 122 eligible studies. The pooled estimate of 1-year survival was 46% (95% CI 43% to 49%; nine population-based studies (n=2408); I2=27%) and 5-year survival was 29% (95% CI 26% to 33%; three population-based studies (n=699); I2=6%).
- In 27 cohort studies, predictors most consistently associated with death were increasing age, decreasing Glasgow Coma Scale score, increasing ICH volume, presence of intraventricular haemorrhage, and deep/infratentorial ICH location. The annual risk of recurrent ICH varied from 1.3% to 7.4% in nine studies and this risk was higher after lobar ICH than non-lobar ICH in two of three hospital-based studies. Four studies reporting the risks of recurrent ICH and ischaemic stroke after ICH found no significant differences between these risks.
Subarachnoid hemorrhage is usually presented with severe sudden headaches, nausea, vomiting, seizures, confusion, and dizziness. About 5 to 10% of these hemorrhages lead to stroke, which is rarely fatal.
Subdural hematoma appears after the trauma to the head caused by an object. This condition can be acute, sub-acute, and chronic, depending on when the symptoms appear. Acute subdural hematoma appears in the first 24 hours, and 50 to 80% of these patients die. Sub-acute and chronic subdural hematoma appear after several days or after 2 weeks from the trauma. The mortality rate for these hematomas is about 20 to 25%.
- www.nhs.uk/conditions/subarachnoid-haemorrhage/
- www.nhs.uk/conditions/brain-aneurysm/
- Photo courtesy of https://www.myupchar.com/en by Wikimedia Commons: commons.wikimedia.org/wiki/File:An_illustration_of_the_different_types_of_brain_hemorrhage.png













Your thoughts on this
Loading...