Every surgical procedure can have many complications, and so can hip replacement surgery. It is a complex surgery, and in most cases, it has a positive outcome. Rarely, there are some complications, and the most frequent complication after hip replacement surgery is blood clots in the legs.
If the blood clot stays in the leg, it is not considered to be a big problem. However, if the clot shifts and starts moving toward the heart and the lungs, it can cause serious consequences. If the blood clot reaches the lungs, it can lead to pulmonary embolism, which is a severe condition with a deadly outcome. Luckily this is a very rare complication. Your doctor can prescribe some drugs which will reduce the chances of blood clot formation.
Some Other Hip Replacement Complications
Another complication that can occur after hip replacement surgery is infection. Infections are caused by bacteria that can get into the body during the surgery. To prevent any kind of bacterial infection, the patient is given antibiotics before and after the procedure. Such safety measures have significantly decreased the number of infections after the surgery.
In some cases, the artificial hip can be infected several years after the replacement. It is usually a consequence of the bacteria which was somewhere else in the body, so the patient needs to receive the proper treatment for infections such as teeth, bladder, or kidney infection before the hip replacement surgery.
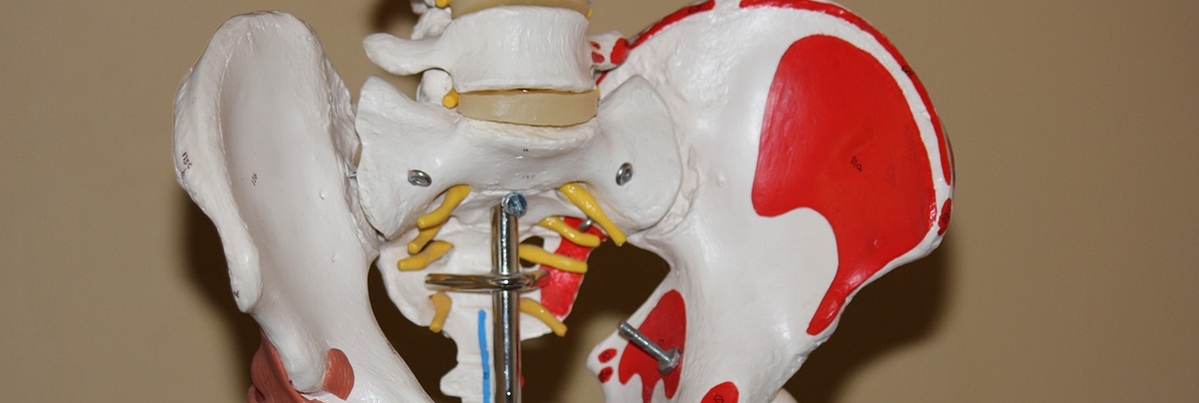
The artificial hip can become loose after some time. This complication depends on many reasons, such as the quality of the surgery and the surgeon who performs it, the quality of the patient's bones (the connection of the artificial hip and your bone will be better if your bones are harder), exercising excessively, being overweight (the more you weigh, the more pressure is placed on the hip), design of the artificial hip and whether the hip is cemented or not.
- Urinary tract infections represent an approximately 13% of all healthcare-associated infection and in the context of post total hip replacement is seen to be the most common minor postoperative compilation.
- Postoperative pulmonary complications are a common complication after total hip replacement with 45.9% patients having some form of postoperative pulmonary complications on postoperative CT screening.
- Deep vein thrombosis is a common complication following total hip replacements due to the venous stasis and hypercoagulability experienced both during and subsequent to the procedure, adversely influencing Virchow’s triad towards a state of thrombus formation.
- Surgical site infections can be classified as that of superficial and deep. Whereas superficial infections can be a nuisance and cause prolonged hospital stays and increased morbidity for patients and potential for wound dehiscence the sequelae of deep infection post total hip replacement can be catastrophic and challenging for the clinician to manage. At the advent of its introduction the deep infection rates for total hip replacements were recorded to be as high as 9.4%. However in modern practice with the widespread adoption of laminar flow operating theatres and prophylaxis antibiotics the current rates of deep infection are at between 0.3 and 1.5%.
- The incidence of nerve injury following a total hip replacement is approximately between 0.05 and 1.9%. Damage to the sciatic and femoral nerve is most common, accounting for 79 and 13% respectively, with combined nerve palsy occurring in 5.8% cases. Obturator nerve palsies are more rare, occurring in 1.6% of cases.
- The rate of hip dislocations can range from 0.2 to 10% with 2% of patients dislocation within 1 year of their operation. Of those who dislocate their total hip replacement, approximately one third will go on to have recurrent dislocations. Risk factors are multifactorial and divided into patient, surgery and implant related.
- Leg length discrepancy following a total hip arthroplasty is one of the most common reasons for patient dissatisfaction as it can cause nerve palsies, abnormal gait, lower back pain and reduced functional outcome. Inevitably this often leads to litigation against orthopaedic surgeons. The incidence has been reported between 1 and 27%. The measured leg length discrepancy have been reported to vary from 3 to 70 mm. As previous covered, nerve palsies are one of the most serious complications of leg length discrepancy. Sciatic and peroneal nerve palsies have both been associated with limb lengthening.
- Heterotopic ossification is the abnormal formation of lamellar bone in extra-skeletal soft tissue. The reported rates of heterotopic ossification post total hip replacement varies greatly between 0.6 and 90%.
















Your thoughts on this
Loading...