Lobectomy
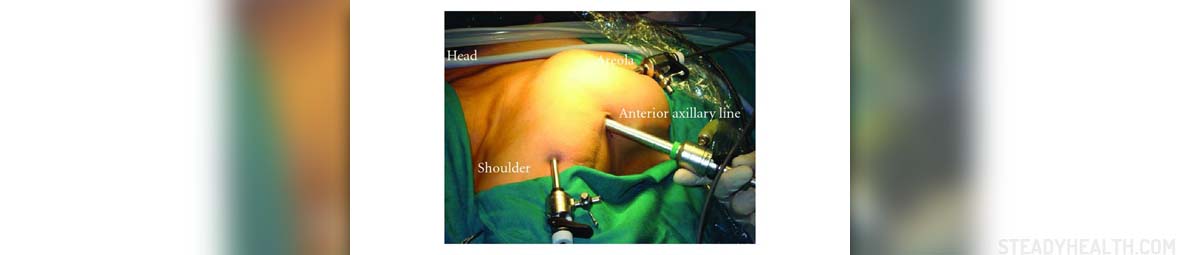
Lobectomy is a surgical procedure in which a pulmonary lobe is resected and removed. This surgical procedure is most commonly performed in people who are suffering from lung cancer. All the possible complications of pulmonary lobectomy may be classified into two groups, minor and major.
Minor Lobectomy Complications
Minor lobectomy complications include nausea and vomiting. These two symptoms are actually a consequence of general anesthesia and they most commonly affect all the patients who have undergone lobectomy. Infection of the incision line and minimal bruising or bleeding may additionally occur.
Numbness of the skin is only a temporary complication and the innervation mostly re-establishes a few months after the surgery. Abnormal scars are also known as keloids can be another minor complication. And finally, a patient may develop an allergy to dressings, tape or latex.
Major Lobectomy Complications
Some patients are more susceptible to complications after lobectomy. General health primarily determines whether a person is going to develop any of the possible complications. People at risk include those suffering from serious heart conditions, kidney disorders, respiratory diseases and diabetes.
Additionally, the risk of severe complications is increased in obese people, heavy smokers and those who have already undergone other surgical procedures. All in all, the most common major complications after lobectomy include continual air leak, bronchopleural fistula, arrhythmia, and injury of the nerves.
After lobectomy the remaining lobe may twist. This leads to its collapse. Even the rest of the lungs can collapse which is another life-threatening complication. And finally, a patient may develop lung failure and die.
As for the heart some of the patients may develop a heart attack. Heart failure is also possible but it is not so common. In some patients, pneumonia or infection of other organs can occur. Heavy bleeding is another complication which if not treated on time can lead to lethal outcome. Even blood clots may form in the blood vessels of the lungs. And finally, a stroke is one more potential complication after lobectomy.
- Prolonged air leak is the most common complication after pulmonary resection, with a reported incidence of 15-18%. Prolonged air leak is defined as a leak lasted more than 7 days after pulmonary resection.
- Pneumonia is a significant concern for thoracic surgeons, with an incidence is reported up to 6% in some studies. Patients are at increased risk after chest surgery for poor pulmonary hygiene, which can lead to the development of atelectasis and progression to pneumonia and/or mucous plugging. Atelectasis causes a ventilation/perfusion mismatch that results in hypoxemia and respiratory decline.
- Atrial fibrillation is the most common arrhythmia following pulmonary resection with an incidence of 10-40% for all pulmonary resections, and 33% for lobectomy. It most commonly occurs on postoperative day 2 or 3, but can occur at any time during recovery. The mechanism of atrial fibrillation after non-cardiac thoracic surgery is unknown, but there are multiple factors associated with developing post-operative atrial fibrillation.
- Postoperative lobar torsion is a rare, but life-threatening complication after pulmonary resection with a prevalence of 0.09-0.4%. Torsion of the right middle lobe (RML) accounts for 70% of cases in the literature.
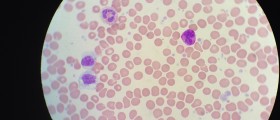
- The incidence of postoperative bleeding after lobectomy requiring at least 4 units of packed red blood cells was found to be 2.9%. If the patient drains greater than 1L in 1 hour or 200mL/hr for 4 hours coagulation labs need to be checked, and, if normal, reexploration is indicated.
- Chylothorax occurs due to injury of the thoracic duct. The incidence of chylothorax with pulmonary resection is 0.7-2%. Aggressive mediastinal lymph node dissection and incomplete ligation of lymph node channels can lead to development of chylothorax.
Lobectomy Aftermath
The problem with patients who have to undergo lobectomy is that majority of them already suffer from some other medical conditions. This way their health is damaged to certain extent and they are actually a risk group for potential complications.
They need to be monitored because only this way a complication can be recognized on time and a patient can be treated timely and adequately. Infections which occur after lobectomy can be easily dealt with antibiotics, excessive blood loss can be restored with blood transfusions and irregular heart beat can be brought under control with antiarrhythmics.
All in all, there are possible complications but by acting properly most of them can be avoided and even if they occur in the majority of cases they can be properly treated.














Your thoughts on this
Loading...