Tyrosine is one of 22 amino acids our body uses to synthesize proteins. As it is the case with any other substance in our body, there is no damage if the level of tyrosine is within optimal range. However, the level of the amino acid may elevate which is medically known as tyrosinemia. The term tyrosinemia is actually used for various disorders. There are three types of tyrosinemia all of which are characterized by an increase in the level of tyrosine. Type I is also known as hereditary infantile tyrosinemia, type II is Richner-Hanhart syndrome while type II has no other name. Transient tyrosinemia of the newborn is one more condition associated with excess of tyrosine but unlike the previously mentioned types it is only a temporary health problem.
Genetic Disorder in the Body
Transient tyrosinemia of the newborn develops due to postponed enzyme maturation in the tyrosine catabolic pathway. This is why this condition is not actually gene related, is considered benign and soon disappears on its own leaving no permanent damage to any part of the body.
On the other hand, all three types of tyrosinemia are gene-related and represent more complex medical conditions. The body of such individuals contain no or only small amounts of the enzymes required for the process of breaking down tyrosine. This results in build-up of both tyrosine and its by-products in various tissues and organs which precipitates serious medical problems. Each type of the disease has distinctive characteristics and is associated with a lack of a specific enzyme.
Type I tyrosinemia develops as a consequence of fumarylacetoacetate hydrolase deficiency. This is the most severe form of the disease with symptoms occurring within the first couple of months after birth. The babies fail to thrive, suffer from vomiting and diarrhea, develop jaundice and are prone to bleeding. They also release a specific cabbage-like odor. This type of the disease is closely connected with liver and kidney failure, damage to the central nervous system and increased risk of cancer development.
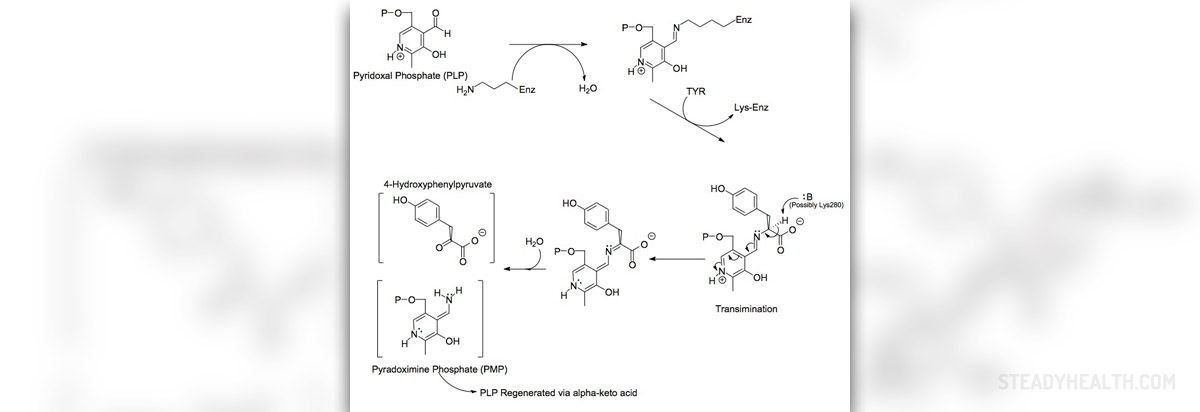
Patients suffering from type II tyrosinemia lack the enzyme tyrosine aminotransferase. Symptoms start in childhood in the form of excessive tearing, photophobia and inflammation of the eyes. Apart from ocular problems these patients additionally suffer from skin lesions (predominantly affecting the palms and soles) and mental health issues. Approximately a half of all patients are intellectually challenged.
And finally, in type III tyrosinemia the body lacks the enzyme 4-hydroxyphenylpyruvate dioxygenase, which in the long run triggers intellectual disability, epilepsy and problems with balance and coordination.
Testing for Tyrosinemia
Patients who are suspected of having tyrosinemia undergo a set of tests and exams.
Initially, blood tests are done. These may reveal normocytic anemia and leukocytosis, both of which are characteristic for the disorder. Some patients additionally have high platelet counts.
Damage to liver cells is accompanied by increased serum bilirubin and transmainase levels. The level of cholesterol is, on the other hand, low. The level of alpha-fetoprotein is also high.
Urinanalysis of these patients show alkaline pH, the excretion of glucose into the urine (glucosuria) and well as loss of proteins in the urine (proteinuria), which are all pathological findings. The urine also contains elevated levels of phosphate and δ-aminolevulinic acid.
Now, when it comes to tests measuring the quality of plasma amino acids, in the beginning they usually reveal selective increase of the level of tyrosine and methionine. Once the liver damage becomes extensive the level of other amino acids increases as well. Tests examining the quantity of amino acids in the urine confirm large amounts of practically all amino acids which is medically known as generalized aminoaciduria. Finally, urinary succinylacetone is the biochemical marker substance which is of major importance for confirming the condition. Its presence in the urine is of crucial diagnostic value for individuals suffering from type I of the disease.
In the end, histological findings may show active inflammation of the liver, lobular regeneration, nodular cirrhosis, fatty infiltration and changes that suggest hepatoma. Tubular swelling and nodules are confirmed after the biopsy of the kidneys is performed.
The majority of patients suffering from tyrosinemia are really ill and they require hospital care. Damage to the liver is sometimes so severe that the primary goal of the treatment is to deal with hepatic decompensation and all the associated health issues such as coagulopaties and other severe complications. Left untreated bleeding may soon result in exsanguination and death.
Doctors try to stabilize patients' health. Severe damage to the liver is an indication for liver transplant surgery, which is the last resort for all patients in whom the organ completely lost its function. Liver transplant is also a treatment option for individuals who have developed hepatic tumor.
During the entire course of treatment the team of doctors including biochemical geneticist, hematologist and hematologist tries to help the patients deal with the disease and manage at least some symptoms. Dieticians play significant role in the treatment as well. They prescribe specific diet low in tyrosine and phenylalanine.
















Your thoughts on this
Loading...