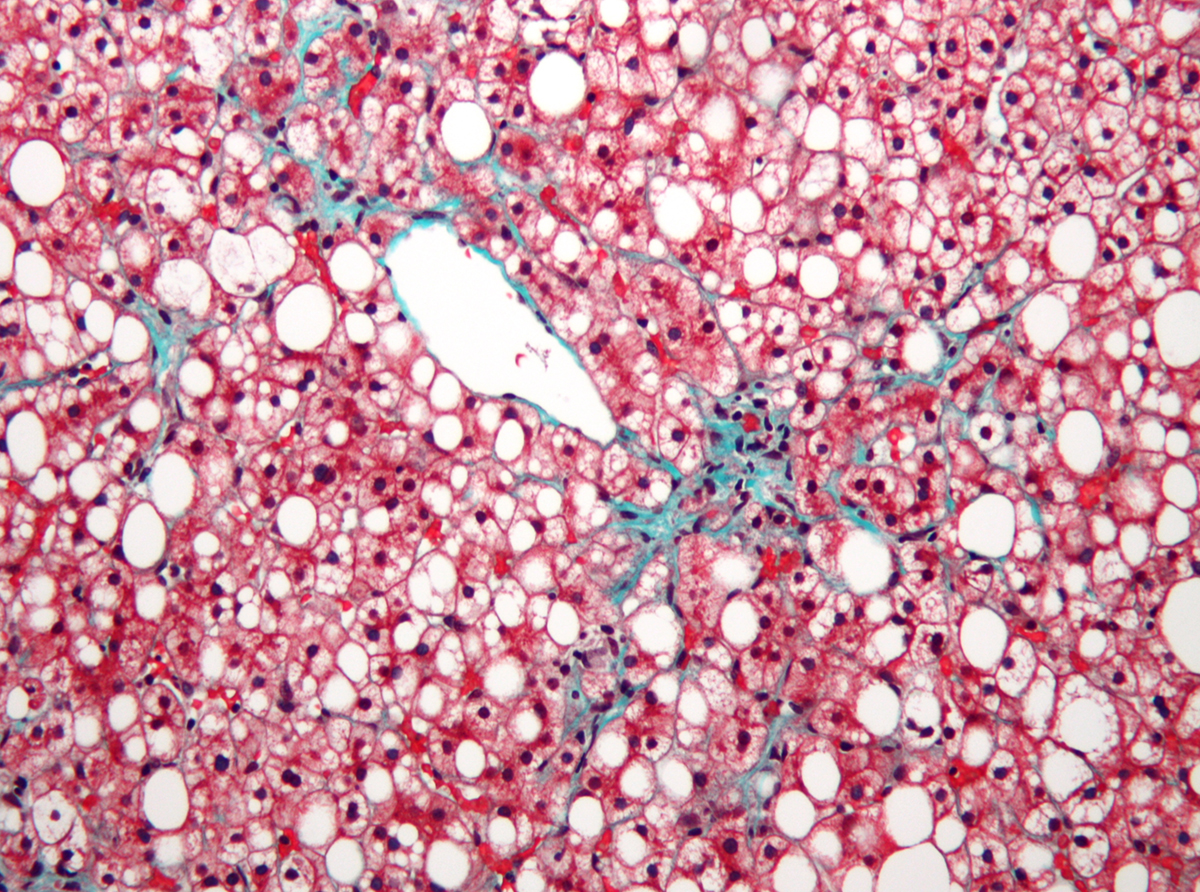
Hepatic encelopathy is a serious complication of advanced stages of liver failure. The condition commonly affects patients suffering from liver cirrhosis and is associated with heavily damaged liver. The organ is simply not able to filter toxins and waste products and the accumulation of such chemicals in the body has detrimental effect on many tissues, organs and organ systems, particularly the brain.
What Causes Hepatic Encelopathy?
The liver is in charge of many functions among which the most significant one is filtering toxic metabolic byproducts.
Hepatic encelopathy develops in people who are suffering from decompensated liver cirrhosis. The damage to the liver is so intensive and toxins accumulate in the blood. Such increased amount of toxins is transferred to the brain. In majority of cases the excess of ammonia is believed to be the most responsible for hepatic encelopathy. Ammonia is a byproduct of proteins. It is normally metabolized into urea and excreted via urine. If there is excess of ammonia there is evident change in function of brain neurotransmitters and consequent changes in patient's behavior. Apart from ammonia there are another substances responsible for hepatic encelopathy and they include short chain fatty acids and mercaptans.
Any factor that contributes to precipitation of nitrogenous waste products in the blood (azotemia) can induce hepatic encelopathy. For example, the condition develops due to consumption of large amounts of proteins and may also occur as a consequence of gastrointestinal bleeding. Furthermore, hepatic encelopathy may affect people with electrolyte imbalance, those suffering from alkalosis, dehydration, constipation, bile duct obstruction etc.
Clinical Characteristics of Hepatic Encelopathy
Hepatic encelopathy features with mild symptoms and signs and in severe cases patients end up in hepatic coma.
Patients commonly suffer from cognitive dysfunction such as lack of concentration, impaired short-term memory, confusion, disorientation etc. Personality, mood and behavioral changes occur as well. There are also motor signs such as muscle tremor (asterixis) and loss of reflexes. In severe cases the person may develop lethargy and stupor. Acute liver failure leads to life-threatening brain swelling.
Apart from symptoms and signs of hepatic encelopathy a patient also develops typical symptoms and signs of decompensated liver cirrhosis such as jaundice, ascites, bleeding varices and gynecomastia.
Treatment for Hepatic Encelopathy
The goal of the treatment is to correct metabolic abnormalities and remove the toxic substances from the body. Furthermore, it is essential to identify the underlying cause of decompensation and bring it under control.
Neutralization of toxins such as ammonia in the intestine is achieved with lactulose. Lactulose may be administered for a longer period of time to patients suffering from hepatic encelopathy. Only in case lactulose is ineffective patients are given antibiotics that are able to reduce the amount of toxins produced by intestinal bacteria. Ammonia can be excreted with the assistance of sodium benzoate and ornithine aspartate. During the attack the diet must be changed and the amount of proteins reduced. Many doctors advise patients to eat more vegetable sources of proteins and to eat foods such as dairy products, fish and chicken than to obtain proteins from meat. Patients who have developed coma require intubation, mechanical respiration and cardiac life support.
















Your thoughts on this
Loading...