Synovial Cysts
Synovial cysts are benign sacs which contain fluid. They typically develop in the facet joints of the lumbar spine and are a consequence of degeneration. Synovial cysts may become large enough to induce spinal stenosis and pressure on spinal nerves. Spinal stenosis causes certain symptoms and requires specific therapy.
Treatment is basically the same as the one applied in case of spinal stenosis. Surgical procedure is required only in those patients who wish to be more active and experience less pain during increased activities. Decompression with a fusion is definitely the most successful surgical approach in treatment of synovial cysts. It provides with significant reduction in pain. This approach is suitable for people who have to deal with mild to severe activity limitations as well as for those suffering from joint instability. It is also an excellent choice for people whose symptoms do not respond to conservative therapy.
Conservative Treatment for Synovial Cysts
There are three treatment modalities for synovial cysts, observation, injections and surgery.
For all patients who do not suffer from pain or have no difficulties related to synovial cyst there is no need for medical treatment. The pain may be induced by certain position and patients may easily deal with pain by changing position which leads to pain.
There are two types on injections administered in patients suffering from synovial cysts. Both of them, facet injections and epidural injections, successfully alleviate the pain. In the first case injections are introduced into the facet joints. The cyst is drained and what follows is injection of steroids. They increase inflammation. Epidural steroid injection technique includes injection of steroids in the epidural space around synovial cyst. This may alleviate the pain but it does not stimulate the reduction of the cyst.
Surgery for Synovial Cysts
In patients suffering from synovial cysts surgeons tend to perform either decompression alone or decompression together with a spine fusion. Microdermocompression of the nerve root and removal of synovial cyst are performed in case there is no accompanying instability. Microdermocompression is minimally invasive surgery and the recovery is rather quick. Unfortunately, synovial cyst may re-form after certain period of time.
Decompression with spine fusion surgery is best possible treatment modality since it includes both, removal of the cyst and fusion of the joint. Fusion of the joint terminates all the motion at that level which consequently does not allow the cyst to regenerate. On the other hand, fusion also creates more stress on other non-fused levels of the spine. This is an open surgery and carries more risk comparing to the previous one. The process of healing lasts approximately 6 to 9 months.
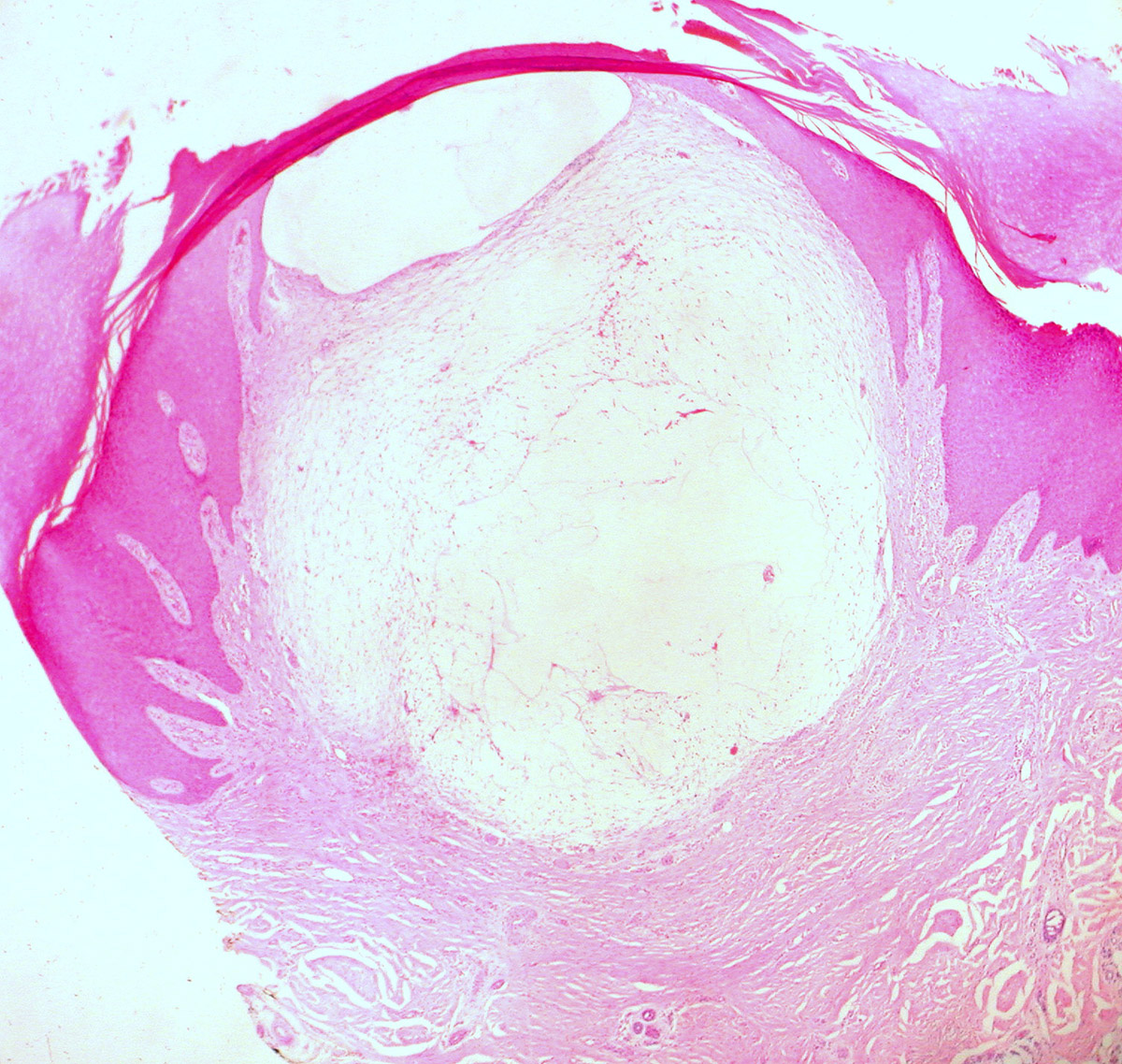
- Lumbar synovial cysts are cystic dilatations of synovial sheaths that directly emanate from facet joints and extrude into the spinal canal. When Tillich et al. correlated magnetic resonance (MR) scans with surgical findings for 18 patients with synovial cysts, the cysts measured an average of 16 mm (ranged 10–28 mm); 3 additionally (17%) contained hemorrhages.
- Two fluid types are found within these cysts. The most common gelatinous cysts are not easily aspirated, while the less frequently encountered serosanguinous cysts, containing less viscous fluid, may be somewhat more amenable to percutaneous aspiration. Nevertheless, whether or not fluid can be removed from within these cysts, the fibrous capsule that remains continues to contribute to the clinically relevant compression of the thecal sac and nerve root.
- Although CT studies more readily diagnose lumbar stenosis and ossification of the yellow ligament (OYL) associated with synovial cysts, MR studies better delineate the severity and extent of the cysts themselves.?
- Utilizing the operating microscope is extremely helpful in avoiding cerebrospinal fluid fistulas during decompression and removal of synovial cysts as these fistulas are more likely to arise secondary to dense adhesions between the cyst capsule and underlying dura/nerve roots. In Epstein's retrospective analysis of 110 predominantly geriatric patients undergoing multilevel laminectomies with non-instrumented fusions, 5 of 10 patients who developed dural tears had attendant synovial cysts. For the 10 patients with dural tears, the average age was 74 years, and they had undergone slightly more extensive laminectomies (average 5.5 levels) and non-instrumented fusions (average 1.8 levels). Notably, all 10 patients exhibited marked OYL that extended to and through the dura in 3 patients. Alternatively, for the 100 patients without dural tears, 8 of whom also had synovial cysts, the average age was a younger 69 years, and they had undergone lesser average 5.0-level laminectomies and 1.6-level non-instrumented fusions.
- Intraoperative somatosensory evoked potential monitoring, electromyographic monitoring, and sphincter monitoring are also useful while resecting synovial cysts. In particular, monitoring these potentials alerts the surgeon to inadvertent, excessive traction that may occur during dissection/manipulation of the cyst away from the underlying thecal sac and/or nerve roots, thereby avoiding permanent injury (e.g. cauda equina syndrome, root and sphincteric deficits).
















Your thoughts on this
Loading...