What is Supraspinatus Tendonitis?
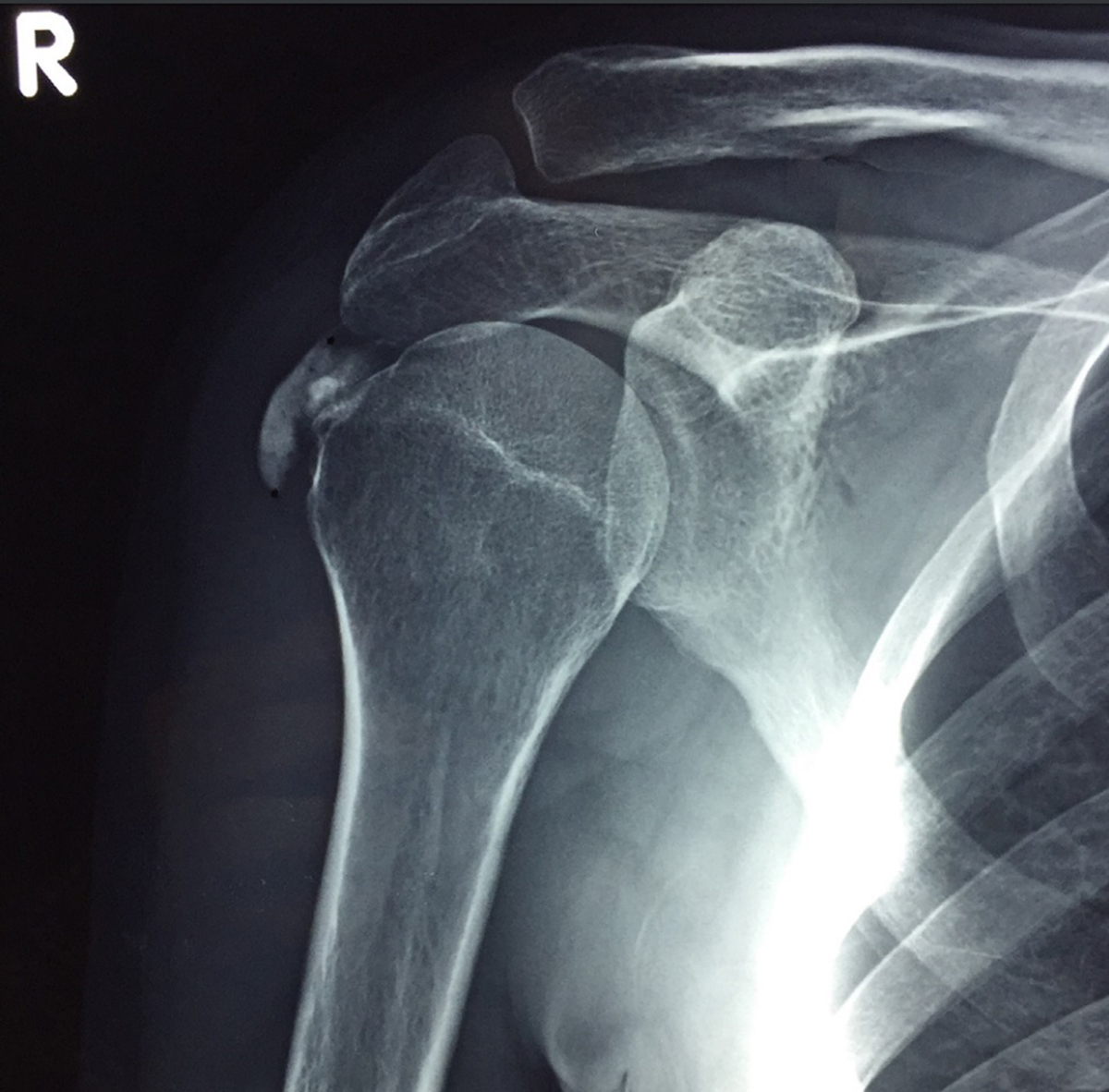
Supraspinatus tendonitis is the Latin for inflammation of the tendons of the rotator cuff, and it is the form of tendonitis that is most commonly treated. The rotator cuff has several tendons. Among these, the supraspinatus tendon, which connects the shoulder blade to the arm bone, is most likely to become inflamed.
The typical cause of supraspinatus tendonitis is repetitive movement. this includes movements associated with playing tennis and a number of other sports that rely on the intensive work of the shoulder muscles and shoulder joints. The pain and discomfort associated with supraspinatus tendonitis can be very intense and even debilitating.
Who is at Risk from Supraspinatus Tendonitis?
Highest risk group includes tennis players and baseball players, with swimmers and golf players at a close second. Certain occupations are also associated with common occurrences of supraspinatus tendonitis. These include carpentry, painting, decorating, and others. The shoulder of the arm that gets used more is more likely to develop supraspinatus tendonitis.
What are the Symptoms of Supraspinatus Tendonitis?
Typical symptom in the early phase is pain and a dull ache in the affected shoulder. Some people will even experience spreading of the pain down the arm or even across the chest. Any movement of the injured arm can cause pain. Putting any kind of load on the shoulder will cause pain, to the extent that sleeping on the injured shoulder becomes impossible due to pain.
If the condition is not treated, the pain will gradually increase to the level that any movement of the arm causes unbearable pain. Most people then avoid moving the arm completely, which leads to stiffness of the shoulder joint (joints that are not regularly used do not lube themselves and become hard to move and painful when moved).
Bruising and swelling around the injured shoulder is also common. So if you use your hands a lot and begin to feel a dull pain in one or both shoulders, do not ignore it, hoping that it will just go away.
Treatment
Whenever possible, treatment is conservative, which means that surgery is avoided if it is not necessary, and treatment is based on physiotherapy and medication by painkillers if necessary.
- Tendon injuries of the rotator cuff (RC) are among the most common problems of the shoulder, affecting people performing sports as well as repetitive activities related to work or daily living.
- Moreover, tendinopathies of the RC increase with aging affecting more than 80% of the people over eighty years of age, with the supraspinatus tendon being the most commonly affected.
- Along with the subscapularis, teres minor, and infraspinatus muscles, the supraspinatus joins to form the RC which functions to compresses the head of the humerus into the glenoid fossa of the scapula.
- The supraspinatus muscle originates from the posterior aspect of the scapula, superior to the scapular spine and inserts on the greater tuberosity of the humerus, blending partially with the tendon of the infraspinatus muscle.
- Anatomically, the insertional supraspinatus tendon is divided into four transitional layered zones according to the extracellular matrix (ECM) content. The first zone is essentially made up of Type I collagen and a small amount of decorin. This zone may be considered the tendon proper. The second zone consists of mainly Types II and III collagen, with small amounts of Types I, IX, and X collagen forming fibrocartilage. The third zone is defined by a mineralized fibrocartilage which is composed by Types II and X collagen, and aggrecan. The fourth zone is formed by Type I collagen, with the collagen fiber orientation defining the effective bone-tendon attachment.
- The model explaining tendinopathy development has been changing over the years. Currently, it is generally accepted that supraspinatus tendinopathy develops when excessive stresses exceed the healing capacity of the tendon cells (tenocytes), with the tendon failing to repair properly.
- Age has been shown to correlate with tendinopathy, having a negative impact on tendon properties, especially after forty years of age. With age, tendons tend to degrade and decrease the ability to withstand tensile loads, and elasticity. Furthermore, in a study with subjects fifty-two years of age and older, Kumanagai et al. have shown that calcifications and fibrovascular proliferation changes, as well as a drop in total glycosaminoglycan and proteoglycan content are present in the aging supraspinatus tendon.
- Therapeutic modalities commonly utilized for tendinopathies may help limit or reverse the degenerative process of tendinopathy by improving repair processes, and by reducing the expression of neovascularity often associated to tendon symptoms. Laser therapy seems to be beneficial and superior to therapeutic ultrasound.
- Over the last several years, exercise in form of eccentric training has been advocated for use with a variety of tendinopathies including Achilles, patellar, wrist extensors, and rotator cuff, with good clinical outcomes. Skillful dosage and implementation of eccentric loading interventions illustrate the important role of the physical therapist in management of tendinopathy with the goal of long term positive functional outcomes.
In cases that were either neglected and the treatment began (too) late, or where conservative treatment does not provide relief, surgery is used as a solution. The type of surgery depends on the cause of inflammation. For example, impingement surgery is used to chip off a small portion of bone from the underside of the outer edge of the shoulder blade, which gives the irritated tendons more space to move.
If the rotator cuff has become torn, then the torn tendons need to be reattached to the upper arm bone. This is done by sewing the tendon to the upper arm bone through the small holes drilled through the bone at the site of tendon attachment. The healing of the tendon is slow as its low blood supply does not provide for quick recovery.















Your thoughts on this
Loading...