Peripheral Blood Circulation
Peripheral blood circulation refers to the blood flow in the legs and arms. Since people usually do not suffer from any problems related to blood circulation in the arms, it is clear that when we discuss problems with peripheral circulation, we actually discuss problems with circulation in the legs.
Impaired peripheral circulation is accompanied by numerous symptoms and signs. Well experienced doctor can set the correct diagnosis after questioning the patient, and performing a physical examination with particular attention to the lower extremities. Several more tests and imaging methods may help in conformation of the condition and can help in visualizing the actual cause of impaired peripheral blood circulation.
Symptoms and Signs of Impaired Peripheral Blood Circulation
The blood from the heart normally reaches all the body organs and organ systems. But, the legs are last supplied. Furthermore, the legs carry the weight of the entire body and are under a lot of stress and pressure. This all has consequences on blood circulation in the legs. Veins are the most susceptible, and they are easily affected by the process of inflammation and structural changes.
Improper functioning of the veins leads to inadequate return of the blood to the heart. The excess of blood leads to further damage of the veins leading to the formation of varices, and the process finally results in permanent problems with peripheral blood circulation. Apart from problems with veins, in some people, arteries are affected by certain inflammatory processes which result in inadequate supply of the legs with the blood.
The initial symptoms of poor peripheral blood circulation are numbness and cramping in the feet and lower legs. The patients may also complain about tingling sensation in the feet and toes. The tingling sensation is generally a consequence of nerve damage.
Swelling is another sign of poor peripheral circulation. The presence of swelling can be easily tested by pressing the lower legs with a finger. If the impression stays for a certain time, one definitely suffers from swelling. Swelling may also be accompanied by increased or reduced temperature of the affected skin.
The temperature of the skin basically depends on whether one is suffering from poor venous or arterial circulation. Inappropriate elimination of the blood from the legs leads to reddening of the skin and other discoloration.
People suffering from poor peripheral circulation also feel tired, and they complain about aches, particularly after standing or sitting for a long period of time. The discomfort can be partially alleviated if one elevates the legs above the level of the heart. This leads to the passive elimination of excess blood and fluids from the legs and relieves the pain.
And finally, in the advanced stage of the disease and neglected cases the skin may suffer serious damage due to insufficient peripheral circulation, and one may develop skin wounds and ulcers. These people also have difficulties when it comes to wound healing.
The process of healing is prolonged and requires special care and additional medical help. These wounds and ulcers are also highly susceptible to infections, which additionally cause even more problems.
- VOP works by creating a system where arterial blood is trapped in a limb segment by inflating occluding cuffs above and below the site under investigation. Proximal (venous occluding) cuffs, placed on the thigh or upper arm, prevent venous blood from leaving the system, and a distal (arterial occluding) cuff, placed above the ankle or wrist, prevents arterial blood from entering the branching vasculature of the foot or hand. Arterial blood flows into the system, while venous flow is halted by the venous occluding cuff, resulting in a condition where blood can enter the extremity but cannot escape. This enables measurement of the accumulating arterial inflow of the investigated limb.
- Measurement of limb blood flow using VOP has clinical relevance, including for the prediction of cardiovascular events and the evaluation of lifestyle and pharmaceutical therapies. In particular, endothelial dysfunction, measured by RH, has been used to evaluate long-term cardiovascular prognosis in patients with PAD. The acute responses to therapy, such as passive heating in patients with PAD, are commonly evaluated using VOP. Furthermore, VOP assessment of endothelial function, measured during states of both RH and active hyperemia, has been used to successfully evaluate the effects of exercise, pharmacological, surgical, and stem cell therapies in patients with PAD.
- During blood flow measurements, the plethysmograph creates a graph showing ‘beat complexes’, where one beat complex corresponds with one cardiac cycle when VOP is simultaneously measured with electrocardiography. This represents the rate and/or rate of change of volume expansion for the area under the strain gauge, which is collectively referred to in the literature as blood flow values.
- medlineplus.gov/ency/article/000170.htm
- www.betterhealth.vic.gov.au/health/conditionsandtreatments/peripheral-vascular-disease
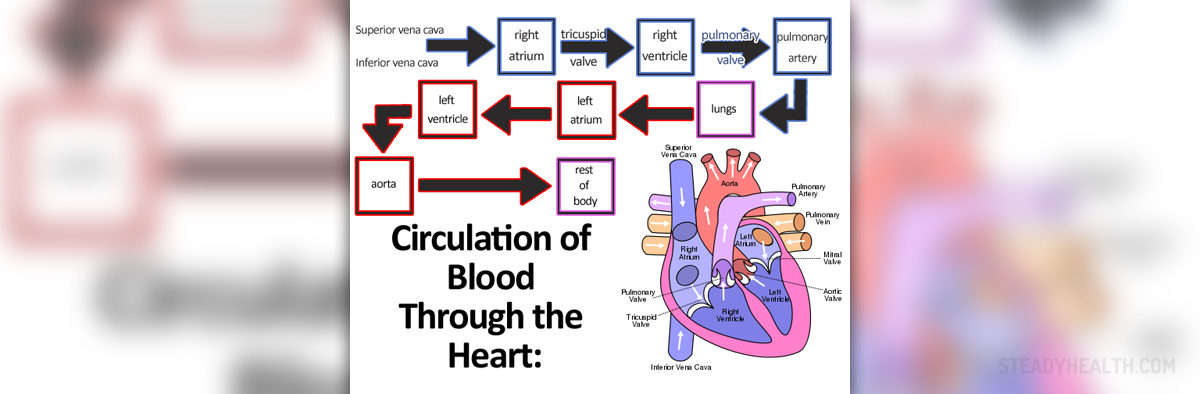
- Photo courtesy of Emibitch by Wikimedia Commons: en.wikipedia.org/wiki/File:Circulation_of_Blood_Through_the_Heart.jpg





_f_280x120.jpg)










Your thoughts on this
Loading...