Definition of Intraventricular Hemorrhage
Intraventricular hemorrhage is by definition bleeding into the brain's ventricular system, the part of the brain in charge of production and further distribution of cerebrospinal fluid. In the majority of cases such bleeding is triggered by physical trauma or develops as a result of a stroke.
Infants are prone to this type of bleeding especially the ones born prematurely or babies with very low birth weight. In infants trauma is not the underlying cause of intraventricular bleeding. On the contrary, their ventricular system is susceptible to any change in perfusion and is likely to suffer from hypoxic ischemic encephalopathy. In case of lack of blood supply, brain cells die, blood vessels decompose and allow blood to leave the circulatory system. In the majority of cases if such bleeding occurs, it is reported within 72 hours after the birth.
As far as adults are concerned, traumatic brain injuries are the leading cause of intraventricular bleeding accounting for 35% of all cases. The prognosis of the bleeding is not so good in individuals in whom the bleeding resulted from hypertension, especially if the entire process is associated with hydrocephalus. Many times there are additional injuries to the brain such as brain contusions or subarachnoid hemorrhage (bleeding in the area between the two membranes surrounding the brain, the arachnoid membrane and the pia matter).
No matter whether intraventricular bleeding affects infants or adult individuals, it is highly dangerous and may easily initiate an increase in intracranial pressure or induce hydrocephalus or irreversible damage to the brain.
Prognosis
Prognosis of intraventricular hemorrhage basically depends on many factors. The amount of lost blood, the type of damage to the nearby brain cells, the overall health of the affected individuals, comorbidities etc.
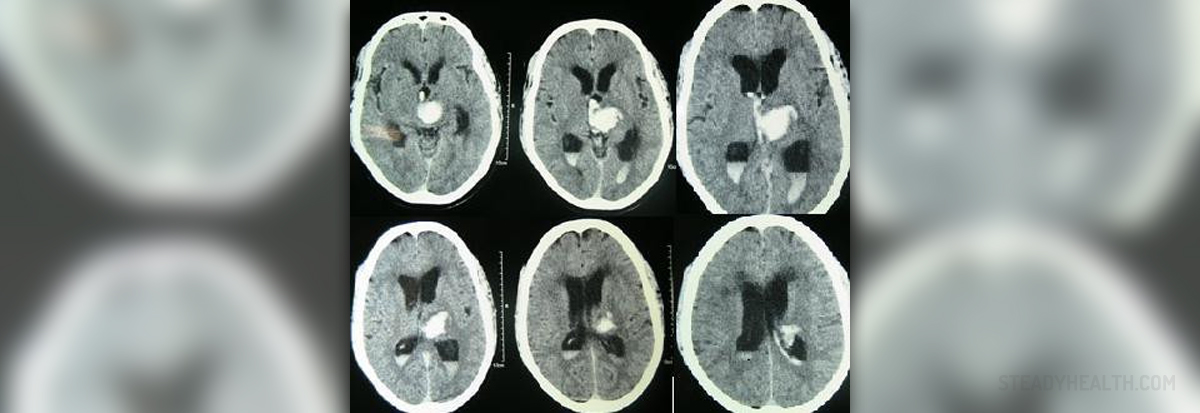
The severity of bleeding can be classified into several grades. In the first grade bleeding is limited only to the germinal matrix. In the second grade there is blood present in the ventricles but they do not change their size i.e. do not expand. Blood in ventricles and their dilation are both characteristic for the third grade of intraventricular bleeding. Finally, in the fourth grade, the blood is found inside the ventricles but it also spreads to the surrounding brain tissue. This grade of intraventricular hemorrhage is actually known as intracranial bleeding because it is distributed in the brain tissue as well.Damage to brain tissue and the ventricular system may be transient. However, not all patients are that lucky because many end up with permanent damage to certain parts of the brain and long-term neurological sequelae.
Permanent complications are a consequence of severe bleeding. For instance, if the person develops grade 1 or 2 intraventricular hemorrhage there may not be any permanent damage. The risk is significantly higher in individuals with the third and fourth grade of intraventricular bleeding when brain cells are directly damaged and may not have a chance to recover.
Management of Intraventricular Hemorrhage
It is simply not possible to stop intraventricular hemorrhage once it begins. So, basically, the treatment is symptomatic, dealing with all the symptoms and signs. Apart from medications and intravenous administration of fluids, patients many times require increased respiratory support.
Hydrocephalus is a common complication of more severe intraventricular bleeding. It is initially treated with medications although if it is irresponsive to medicamentous treatment, the patients require surgery. Most of the times surgeons perform ventriculoperitoneal shunting, surgery that allows the excess of cerebrospinal fluid to be drained into the peritoneal cavity. This surgery efficiently reduces the increased intracranial pressure. Supporting care is also in a form of treatment of potential coagulopathies and circulatory issues.
Many health experts are trying to find the ways efficient enough to prevent intraventricular hemorrhage from occurring.
When it comes to intraventricular hemorrhage in infants, it can be successfully prevented if all the babies are born within the optimal term. By preventing preterm births, the number of such bleeding can drastically decrease. There have been some studies investigating drugs that may be beneficial for mothers at risk of preterm delivery which may be capable of preventing intraventricular bleeding. Steroids and Indomethacin have been involved in this investigation so far.
In adults it may be possible to prevent intraventricular bleeding only if people would take care of their health and prevent all the underlying conditions that may trigger such bleeding. Atherosclerosis, high blood pressure, diabetes and many more conditions may be avoided and if they do not occur, the risk of bleeding into the brain's ventricles significantly decreases. Injuries to the head, another cause of the aforementioned bleeding can also be sometimes prevented. Still, there is no definitive way of complete and utter prevention of such bleeding.
Additional Data
According to the available data, the amount of the blood inside the affected ventricles correlates with the degree of the damage and likelihood of the survivals. It additionally affects complications and long-term sequelae. Therefore, it is of major importance to engage any available treatment in order to limit inflammation, edema, and cell death. The goal is also to restore normal cerebrospinal fluid flow.
- Intraventricular hemorrhage can be a devastating consequence of intracerebral hemorrhage, in adults, and germinal matrix hemorrhage, in premature infants.
- There are a number of potential strategies to try and limit the occurrence and size of IVH including targeting cerebrovascular remodeling and stability.
- Intraventricular hemorrhage results in a physical disruption that is a target of hematoma evacuation and efforts to accelerate hematoma resolution pharmacologically.
- Intraventricular hemorrhage also causes secondary injury via the release of factors from the hematoma that induce damage, neuroinflammation and cause cerebrospinal fluid hypersecretion.
- Such factors include hemoglobin, iron and thrombin. These factors (or their downstream mediators) may be therapeutic targets for reducing IVH-induced brain injury.
- Improving brain recovery after IVH is also a therapeutic target, e.g. via stem cells.














Your thoughts on this
Loading...