Definition and Purpose
Lumbar puncture is a medical procedure that includes insertion of a needle into the subarachnoid space in the area of lumbar spine. This way the cerebrospinal liquid is obtained and can be further investigated. Basically the lumbar puncture is done in case that doctor suspect on meningitis. It can be also performed to confirm or rule out other conditions such as subarachnoid bleeding, hydrocephalus or benign intracranial hypertension.
The placement of the needle into the subarachnoid space is very convenient for administration of certain drugs such as chemotherapeutics in case of certain cancers. This pathway is also used when spinal anesthesia is administered.

Contraindications
In case of intracranial pressure whose precise cause has not been established lumbar puncture is a contraindication. So before each and every lumbar puncture it is best to perform CT scan of the brain and spine. Sometimes increased intracranial pressure can be reduced by lumbar puncture but the real cause of the increased pressure may be a tumor which can after the puncture lead to herniation of the brain in foramen magnum and instant death. In cases like this CT scan is perfect in modification of treatment options.
In coagulopathies, difficulties with breathing as well as in case of increased blood pressure this procedure in a contraindication. Even deformities of the back such as scoliosis and kyphosis can impede in the procedure unless the doctor is experienced enough.
Complications of Lumbar Puncture
The standard complication better to say consequence of lumbar puncture is headache. The headache can be effectively treated with analgesic medications together with intravenous fluids. The best prevention of this complication is maintained supine posture after the lumbar puncture. The patient is advised to stay in this position for approximately two hours.
The patient should rest in bed and if the headache continues and is even more intensive in sitting position there may be additional complication - the leakage of the cerebrospinal fluid from the place of punction. This complication is treated by an epidural blood patch. This patch is actually patient's blood which is injected into the leaking spot. The blood coagulates and stops the bleeding.
- The risk of complications was studied in a cohort of 376 patients who underwent lumbar puncture for evaluation of acute cerebrovascular disease. The following frequency of complications was noted: backache (25 percent), headache (22 percent), headache and backache (12 percent), severe radicular pain (15 percent), and paraparesis (1.5 percent). Severe pain or paraparesis occurred in 6.7 percent of patients receiving anticoagulants following the procedure and in none of the 34 patients who did not receive anticoagulants.
- Headache, which occurs in 10 to 30 percent of patients, is one of the most common complications following lumbar puncture. Post-LP headache is caused by leakage of cerebrospinal fluid (CSF) from the dura and traction on pain-sensitive structures. Patients characteristically present with frontal or occipital headache within 24 to 48 hours of the procedure, which is exacerbated in an upright position and improved in the supine position. Associated symptoms may include nausea, vomiting, dizziness, tinnitus, and visual changes.
- Infections are rare after lumbar puncture; in typical patients no techniques beyond usual aseptic technique are required. Meningitis is an uncommon complication of lumbar puncture. In a review of 179 cases of post-LP meningitis reported in the medical literature between 1952 and 2005, half of all cases occurred after spinal anesthesia; only 9 percent occurred after diagnostic lumbar puncture. The most commonly isolated causative organisms were Streptococcus salivarius (30 percent), Streptococcus viridans (29 percent), alpha-hemolytic strep (11 percent), Staphylococcus aureus (9 percent), and Pseudomonas aeruginosa (8 percent).
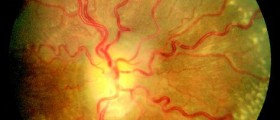
- Bleeding - The cerebrospinal fluid is normally acellular, although up to five red blood cells (RBCs) are considered normal after lumbar puncture due to incidental trauma to a capillary or venule. A higher number of RBCs is seen in some patients in whom calculation of the white blood cell (WBC)-to-RBC ratio and the presence or absence of xanthochromia may differentiate LP-induced from true central nervous system (CNS) bleeding.
- Serious bleeding that results in spinal cord compromise is rare in the absence of bleeding risk. Patients who have thrombocytopenia or other bleeding disorders or those who received anticoagulant therapy prior to or immediately after undergoing lumbar puncture have an increased risk of bleeding. This risk may be further increased with other factors that increase bleeding risk, such as traumatic or repeated taps.
One more complications results from the needle which can get in touch with the roots of spinal nerves and lead to abnormal sensations. These sensations affect lower extremities and are transient.
Severe complications such as epidural or spinal hemorrhage are not so common. The injury to the spinal nerves can lead to paraplegia in most extreme cases of possible complications.
In case there is slightest doubt about possible presence of epidural infection the intervention is not done. Even in cases of skin infection at the spot of puncture the intervention is avoided.






_f_280x120.jpg)








Your thoughts on this
Loading...