Upper gastrointestinal endoscopy is a diagnostic procedure done to assess the conditions affecting the upper parts of the gastrointestinal tract. Complications due to this method are rather rare. All the complications may be divided into cardiopulmonary complications, complications due to sedation, infections, perforation within the gastrointestinal tract, and hemorrhage.
Cardiopulmonary complications occur mainly because of the anesthesia which is regularly administered during the endoscopy. Out of all complications, these are the most usual during endoscopy. They feature slight changes in vital signs and even can present with myocardial infarction and breathing depression. Shock due to hypotension may develop as well.

However, all of the previously mentioned complications are much more common for people who already suffer from cardiac and pulmonary diseases. They are also more frequent in elderly patients. Today conscious sedation is applied more, and constant monitoring prevents certain complications from developing. In the case of cardiopulmonary arrest, the methods of resuscitation are performed. All the medications that may be needed are at the doctor's hand.
The infections after the procedure may be caused by the procedure itself or the infective agents which may contaminate the equipment. There is the possibility of transitory bacteriemia during the endoscopy. In rather rare cases, bacterial endocarditis may occur as one pretty serious complication of the procedure. This is why in some cases antibiotics are administered as a method of prophylaxis.
In extreme cases, retropharyngeal or retro esophageal abscesses may develop. The equipment is regularly sterilized so the possibility of contamination is reduced to a minimum.
Perforation
One of the serious complications includes perforation. This does not happen often but can be severe. One of the factors that may predispose to this complication is the presence of anterior cervical osteophytes. Zenger’s diverticulum is a condition that makes the wall of the pharynx or esophagus thinner hence the place of the change is more susceptible to perforation.
Esophageal strictures and malignancies of the upper gastrointestinal tract may also be the cornerstone for perforation. In the case of esophageal perforation, the rate of lethal outcome is around 25%. The state features pain in the chest, fever, and an increased number of white blood cells.
If the air from the gastrointestinal tract comes into the peritoneum it can be identified by a plain radiograph of the abdomen. The prognosis of this complication basically depends on the place of perforation and the overall health of the patient.
Bleeding
Bleeding may also occur during the gastrointestinal endoscopy. Extreme bleeding is not so common. The individuals prone to bleeding are those suffering from thrombocytopenia and coagulopathy. All the biopsies are taken with precautions.
- The rate of cardiopulmonary adverse events in large, national studies is between 1 in 170 and 1 in 10,000. Reported adverse events range from minor incidents, such as changes in oxygen saturation or heart rate, to significant adverse events such as aspiration pneumonia, respiratory arrest, myocardial infarction, stroke, and shock.
- Infectious adverse events of diagnostic UGI endoscopy can result from either the procedure itself or failure to follow guidelines for the reprocessing and use of endoscopic devices and accessories.
- Prospective, multicenter registries report perforation rates of 1 in 2500 to 1 in 11,000. Factors predisposing to perforation include the presence of anterior cervical osteophytes, Zenker’s diverticulum, esophageal stricture, malignancies of the UGI tract, and duodenal diverticula. Perforation of the esophagus is associated with a mortality rate between 2% and 36%.
- Clinically significant bleeding is a rare adverse event of diagnostic UGI endoscopy. Mallory-Weiss tears occur in less than 0.5% of diagnostic UGI endoscopic procedures and usually are not associated with significant bleeding. Bleeding may be more likely in individuals with thrombocytopenia and/or coagulopathy.
- Data from randomized trials and large case series suggest that the overall rate of dilation adverse events is between 0.1% and 0.4%. The most common adverse events are perforation, hemorrhage, aspiration, and bacteremia. Most dilation-related bleeding is self-limited, but rare episodes of bleeding requiring endoscopic hemostasis and dissection into major blood vessels have been reported.
- Many of the adverse events associated with endoluminal therapy can be treated endoscopically. Bleeding can be controlled with injection hemostasis, APC, hemostatic graspers, or endoscopic clips. The risk of delayed bleeding after EMR may be reduced by prophylactic closure of mucosal defects with endoscopic clips. High-dose proton pump inhibitor therapy improves ulcer healing rates and reduces the risk of delayed bleeding after ESD.
- www.nhs.uk/conditions/endoscopy/
- www.nhs.uk/conditions/gastroscopy/
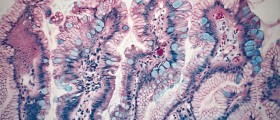
- Photo courtesy of Yuya Tamai by Flickr: www.flickr.com/photos/tamaiyuya/180619506
















Your thoughts on this
Loading...