What is Esophagogastroduodenoscopy?
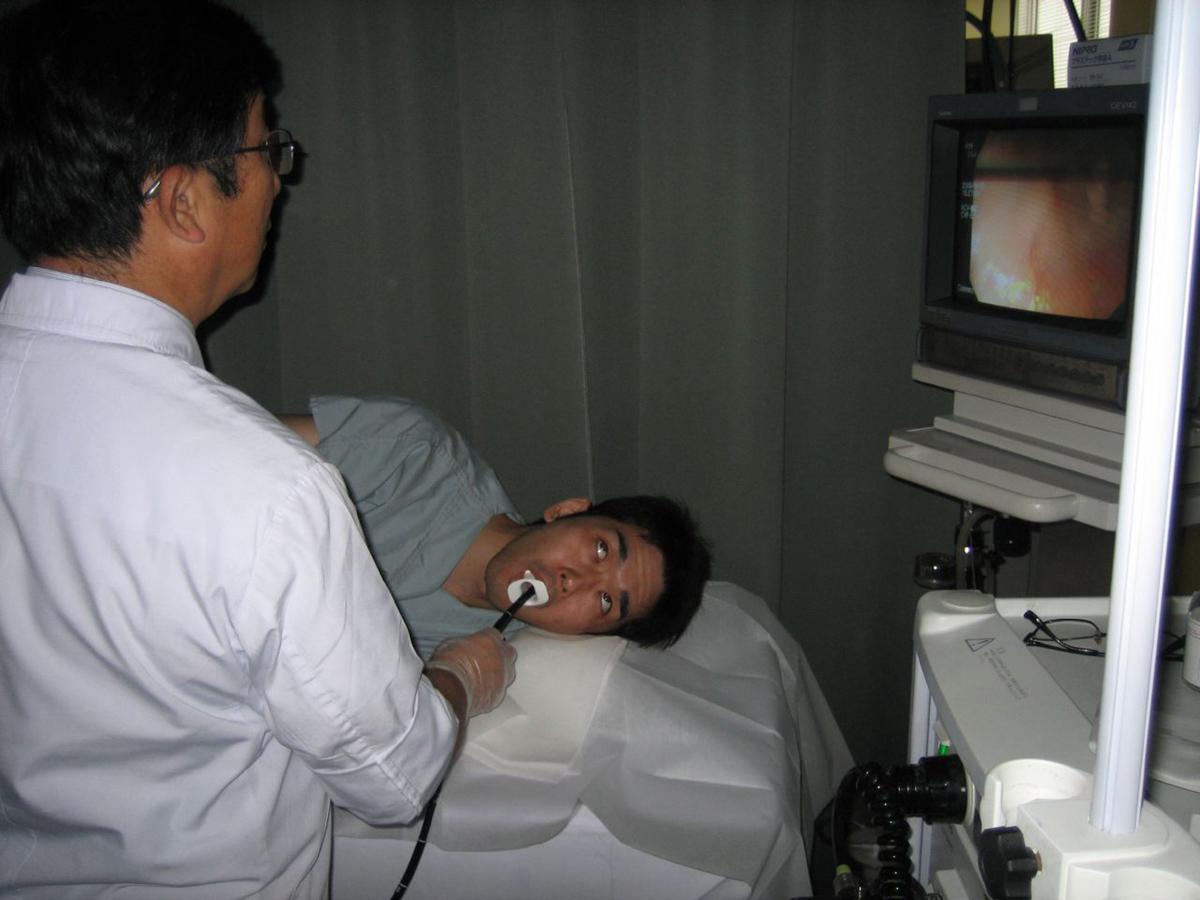
Esophagogastroduodenoscopy is also called upper endoscopy, upper gastrointestinal endoscopy, or short EGD. That is a diagnostic procedure that involves a small flexible camera (endoscope) introduced through the mouth to examine the lining of the esophagus, stomach, and upper duodenum.
Purpose of EGD
Esophagogastroduodenoscopy is used for both diagnostic and therapeutic procedures. If you suffer from symptoms connected to the upper gastrointestinal tract, upper endoscopy will probably be necessary. Such symptoms include pain localized in the chest or upper stomach, nausea or vomiting, gastroesophageal reflux disease (GERD), trouble swallowing or dysphagia, and bleeding from the upper intestinal tract.
Upper gastrointestinal endoscopy can be used for therapeutic interventions such as control of bleeding, ablation of neoplasms, gastrostomy placement, removal of polyps or other non-cancerous tissues, dilation or stenting of stricture, and retrieval of foreign bodies.
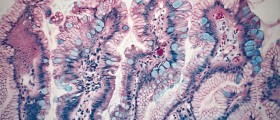
EGD is used for taking samples (biopsies) for suggested gastrointestinal (GI) diseases, such as malabsorption, infections, or neoplasms. When inflammation, ulcer, or tumor is suspected, upper endoscopy is more reliable than X-ray.
To be precise, disorders that are identified, evaluated, and treated with the use of upper endoscopy include Crohn’s disease, cancer of the esophagus, gastroesophageal reflux disease, rectal bleeding, stomach cancer, irritable bowel syndrome, stomach ulcers, and hiatal hernia.
EGD Procedure
Esophagogastroduodenoscopy procedure performed by a gastroenterologist. The patient receives sedatives and painkillers. Local anesthetic is sprayed in the patient’s mouth, and he or she is instructed to lie on his left side. The endoscope is then advanced through the esophagus to the stomach and duodenum (part of the small intestine).
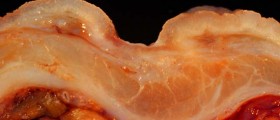
Camera at the end of the endoscope sends images to a monitor, thus allowing the endoscopist to look at the entire upper gastrointestinal tract. If needed, biopsies can be taken through the endoscope. Different treatments can be performed as well.
Contraindications
EGD is contraindicated in patients suffering from severe upper gastrointestinal (UGI) bleeding. Contraindications also include possible perforation, unstable patients, or unwilling patients. Upper gastrointestinal endoscopy shouldn’t be performed on patients with a history of bleeding disorders such as pallet dysfunction or hemophilia esophageal diverticula. Apart from that, EGD shouldn’t be performed on patients who recently had surgery on the upper gastrointestinal tract.
Complications
EGD is generally done with successful results and very limited complications. The rate of complications of esophagogastroduodenoscopy is less than 2%. Minor complications of upper endoscopy include nausea and vomiting, reaction to medication, and allergic skin reaction. Severe complications are related to the heart or lungs. This includes pneumonia, irregular heart rhythms, and lung or heart failure. Sometimes perforation and bleeding can occur as well. Infections rarely occur as a result of EGD.
- Prevention of complications can be optimally achieved through appropriate patient selection and fostering a safe team working environment.
- Cardiopulmonary-related events account for over 60% of unplanned events during endoscopy and can be minimised by safe sedation and preprocedure risk assessment.
- Early recognition and prompt management is essential to minimise downstream harm once a complication has occurred.
- Management of a complication is often multidisciplinary requiring early involvement of surgical and radiological teams.
- Reporting of complications through departmental meetings and audits is essential and includes a timely apology and duty of candour letter.
- Mechanisms for debriefing, learning and professional support should be available to clinicians involved in a procedure-related complication.














Your thoughts on this
Loading...