Coronary artery bypass surgery is a highly effective method in relieving angina and reducing the risk of death from coronary artery disease. This surgical procedure helps to relieve chest pain, reduces fatigue, and may even increase the ability to exercise while reducing the reliance on medications.
Risks and Benefits
This is a fairly safe procedure, and for an otherwise normally functioning patient, there are no conditions that could make the surgery risky. The associated risk of death is less than 1%. However, there is a slight chance of a heart attack during the surgery, because it is usually performed with the heart stopped. The risk factor associated with this complication is about 5%.
On the other hand, patients who already had a heart attack or other cardiovascular problems before, may be at increased risk of repeated heart attacks. As much as 90% of patients who undergo this surgery report a complete or serious relief of their symptoms. For most of them, it is a life-saving procedure.
Causes
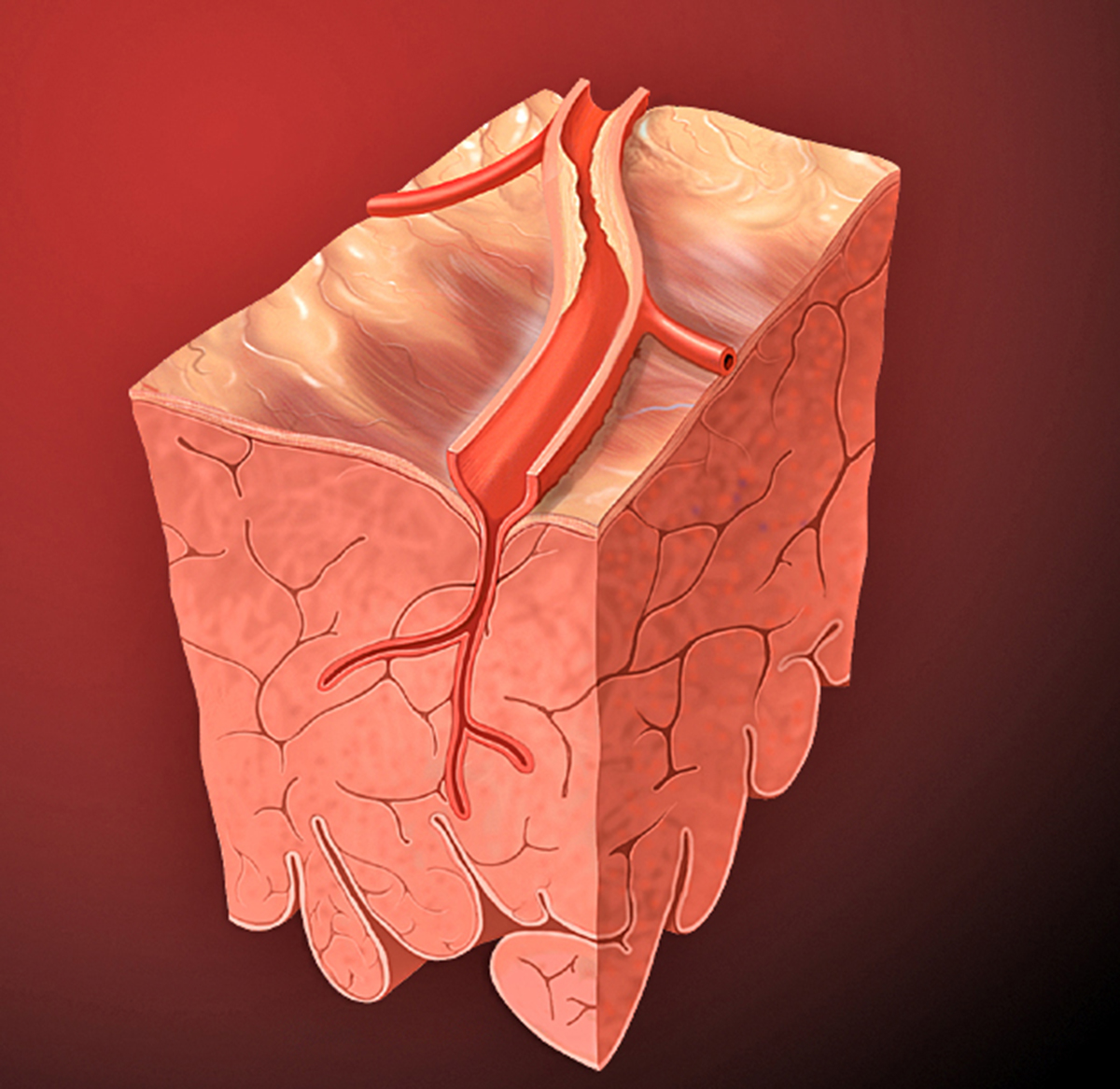
Coronary artery bypass surgery is conducted on patients suffering from a serious form of coronary artery disease. This is a condition in which fatty cholesterol plaque builds up inside the coronary arteries, narrowing them and reducing the blood flow to the heart muscle. Plaque can also facilitate the formation of blood clots or thrombosis. Blood clots may form inside the arteries and partially or chunk the blood circulation to the heart muscle.
Two types of blockage occur in the bloodstream. The first kind is a partial blockage that most commonly results in chest pain or angina. It occurs because the heart muscle is not getting enough oxygen. Patients suffering from angina may also need to undergo coronary artery bypass surgery. Angina is most commonly caused by coronary artery disease.
The second type of blockage that occurs in the bloodstream is a complete or total blockage. If this kind of blockage happens, the heart muscle is not getting any oxygen from the blood flow, and its cells are gradually starting to die. This state is known as myocardial infarction or heart attack.
Diagnosis
Coronary artery disease is diagnosed based on symptoms and examinations. Doctors usually perform physical examinations and blood tests. The most commonly used diagnostic tools are the exercise stress test, a cardiac nuclear scan, and cardiac catheterization. Based on the outcome of this analysis, a doctor will decide if the patient is suited for a coronary artery bypass surgery.
- Coronary revascularization procedures via surgical revascularization are common and costly.
- Despite consideration for increased use of arterial grafts, saphenous vein grafts remain the most commonly used conduits in practice.
- The need for percutaneous intervention to bypass grafts is common and consideration for native vessel versus graft intervention is multi-faceted.
- Coronary revascularization through either percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) remains one of the most frequently performed and costly procedures in the United States, with costs exceeding $6.7 billion annually in Medicare inpatient payments. CABG remains the standard of revascularization for patients with multi-vessel disease, left main disease, and systolic dysfunction. Procedural volumes in the United States alone are around 200,000 CABG cases and 500,000 PCIs are performed annually.
- Choosing appropriate bypass conduits is important in consideration of long-term outcomes after surgical revascularization. There has been renewed interest in arterial revascularization including the use of bilateral internal thoracic arteries or radial arteries as conduits; however, these still comprise only a small subset of procedures [4.9% and 6.5% of secondary graft choice following the internal mammary artery (IMA)].
- Atherosclerotic coronary artery disease, the resultant ischemic cardiomyopathy, and related sequela comprise the leading cause of death worldwide and is not projected to diminish in the foreseeable future. Therefore, medical professionals involved in percutaneous and surgical coronary revascularization will continue to discuss, study, and reassess the efficacy and overall impact on survival and quality of life of many of the topics highlighted in this publication.
- medlineplus.gov/ency/article/002946.htm
- www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/heart-bypass-surgery
- Photo courtesy of Patrick J. Lynch, medical illustrator by Wikimedia Commons: commons.wikimedia.org/wiki/File:Heart_coronary_artery_lesion.jpg
















Your thoughts on this
Loading...