Colostomy is a name of a surgical procedure which manifests through one part of the large intestine being attached to the abdominal wall. Through an opening created on the abdominal wall, a bag is connected to the large intestine, collecting all the waste material. This bag is called colostomy bag.
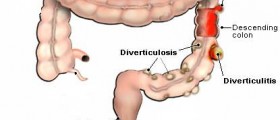
This process is necessary in order to allow one's colon enough time to recuperate after a cancer surgery. Also, colostomy can help people heal from illnesses such as diverticulitis or bowel obstruction.
Depending on the health of the patient, this procedure can be reversible or permanent. The former procedure involves reconnecting the large intestine to the rectum through colostomy takedown.

The Colostomy Takedown Procedure
There are two ways of performing both the colostomy and its reversal surgery. The first is open surgery, carried out after a large incision has been created. Secondly, a more common variant, is laparoscopic surgery where several smaller incisions are made, allowing the laparoscopic instrument to be inserted.
During colostomy takedown, the abdominal wall is lifted and the large intestine is disconnected from it, only to be reconnected to the rectum by a special, stapling device. Once the whole process is done, the incisions are sutured or stitched and the spot is covered by bandages.
- All patients receive a preoperative bowel preparation and an enema to evacuate the rectal stump. The patients are placed in the modified lithotomy position and a three-way Foley catheter is placed.
- Port placement is related to the location of the prior abdominal incisions and the stoma. Either the colostomy site is used or an open cut down technique is performed to access the peritoneal cavity. If the prior midline incision extends to the epigastrium, the initial port is placed at the colostomy site. The colostomy is mobilized and the most distal segment of the colostomy is transected with a stapler at the mucocutaneous junction. The stapled colon is dropped back into the abdomen and a 10 mm balloon tipped trocar is placed in the prior colostomy site.
- If a lower midline incision is present, initial access to the peritoneal cavity is typically gained with an open technique under direct vision in the left upper quadrant. A 5- or 10 mm port is placed in this incision. Typically, three ports are used in total with the third being located to the left of the midline superiorly. The benefit of these port placements is that the dense adhesions frequently found along the prior midline incision can be avoided and adhesiolysis minimized.
- Sharp adhesiolysis is performed to mobilize the splenic flexure and left colon. Excessive adhesiolysis of the prior midline incision is avoided. Next, the rectal stump is identified. If polypropylene sutures were placed on the rectum at the time of initial operation, they can greatly aid in the localization of the rectal stump.
- Mobilization of the splenic flexure in an open technique requires a larger midline incision, which can lead to an increased risk of postoperative morbidity. Splenic flexure mobilization is required often for this operation to reduce tension on the anastomosis with its resultant anastamotic dehiscence or stricture formation.
- Avoiding the previous midline incision by accessing the abdomen laterally can help prevent the possibility of bowel injury. In our cases, the abdomen is always entered at a site remote from prior incisions. Keeping our ports on the left side of the body, the midline is often completely avoided. By doing this we have had no visceral injuries in our series.
What Can Go Wrong During Colostomy Takedown?
Colostomy and its reversal procedure both can stumble upon certain complications. Therefore, following the doctors and the surgeons instructions is crucial, both before and after the surgery. In most cases, lack of proper connection of the large intestine can lead to leakage due to improper healing of the spot. If not treated immediately, this exposure to waste material can result in a life-threatening infection. Thus, an additional surgery is usually a must in these cases, even though some occurrences of this problem can be dealt with by antibiotics.
Quite often, people who have undergone colostomy takedown face bowel movement problems, inconsistence, nausea or infections. In some rare cases, they may even develop an allergic reaction to the anesthetics used. Sometimes, the intestine can bulge out into a weak spot created during the abdominal wall surgery. Once this hernia appears, it needs to be dealt with through yet another surgery.
Fortunately, if you follow all the instructions your surgeon has given you, you have increased chances of surviving colostomy takedown without any complications. You will need to modify your diet, restraining yourself from consuming certain types of food and pay close attention to your health, seeking medical assistance if you notice some negative occurrences.















Your thoughts on this
Loading...