The endometrium is a mucous membrane that lines the inner surface of the uterus. During the reproductive period, the endometrium normally changes its thickness due to hormones, and depending on the phase of the menstrual cycle, it may be thin or become thicker. However, in some cases, thickened endometrium is not considered normal, especially if the cause of thickening is endometrial hyperplasia.
Pathological Thickened Endometrium
Endometrial hyperplasia or thickened endometrium is a medical condition that features excessive proliferation of the endometrial cells. In the majority of cases, endometrial hyperplasia is caused by elevated levels of estrogens and low levels of progesterone.
This typically occurs in certain gynecological illnesses such as polycystic ovary syndrome, estrogen-producing tumors, and in the case of estrogen replacement therapy. Endometrial hyperplasia must be taken seriously and treated properly and timely since it represents a risk factor for endometrial cancer.
Classification of Thickened Endometrium
Thickened endometrium or endometrial hyperplasia is a physiological response of the endometrium to estrogen. There are several subtypes of endometrial hyperplasia, which are classified according to their pathophysiological characteristics.
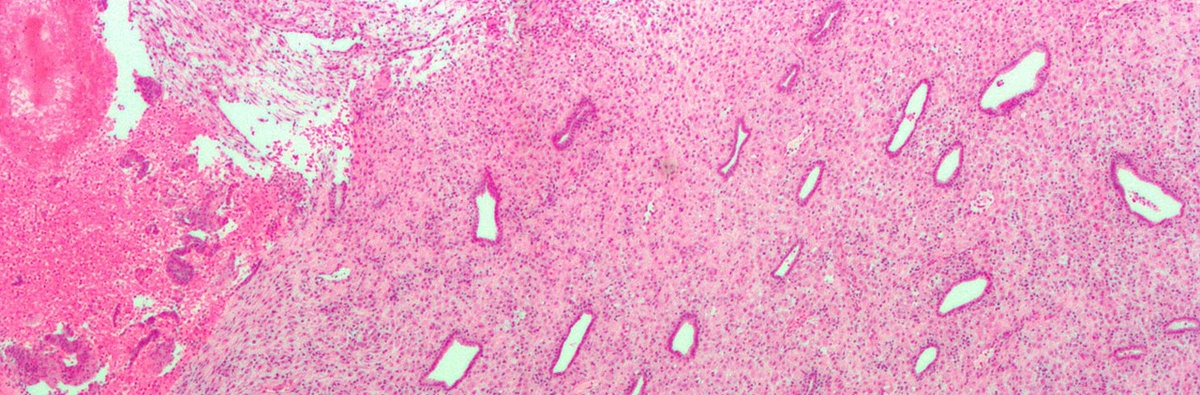
Simplex or complex endometrial hyperplasia represents irregularity and cystic expansion or budding of endometrial glands. There are no bothersome changes in the appearance of the glands.
Simplex or complex atypical endometrial hyperplasia features with bothersome architectural changes in gland cells. These changes include cell stratification, tufting, loss of nuclear polarity, enlarged nuclei, and increased mitotic activity. All of the previously mentioned makes atypical endometrial hyperplasia a precancerous condition that eventually turns into actual invasive endometrial cancer. In atypical endometrial hyperplasia, there is no invasion of the connective tissue.
- The number of new EC cases in Europe in 2018 was 121,578, with 29,638 deaths. Individual risk factors related to the development of EC are nulliparity, obesity, polycystic ovary syndrome, early menarche, and late menopause.
- Women with hereditary nonpolyposis colorectal cancer syndrome have an estimated cumulative incidence of EC of 20%–60% by the age of 70 years. Although most EC is diagnosed in menopause, 5%–30% of cases are diagnosed in premenopause, with a risk of 1.33%.
- In premenopausal women, the utility of TVUS for excluding malignant endometrial abnormalities has not been established. Few data are available on the efficacy of ET measurement in premenopausal women with abnormal uterine bleeding (AUB). This cohort of patients is subject to cyclic modification of the endometrium, due to the hormonal cycle. The best time to perform TVUS is on days 4–6 of the menstrual cycle, when ET should be as its thinnest.
- Ozdemir et al evaluated ET in 144 premenopausal women with AUB, reporting that ET ?8 mm showed the best sensitivity and specificity for endometrial abnormality screening, considering both benign and malignant conditions. Endometrial hyperplasia and cancer were diagnosed respectively in 11.8% and 5.5% of patients, and the endometrium was thicker in patients with endometrial hyperplasia (12.71±4.24mm) and EC (15.25±8.23mm).
- One of the biggest studies published, performed by Kim et al in South Korea, studied a group of 9888 women to determine clinical factors and sonographic findings associated with endometrial hyperplasia or cancer in premenopausal and perimenopausal women. Only endometrial echo abnormality had a significant association with endometrial hyperplasia. There was no significant association between ET and endometrial malignancy or premalignancy lesions.
- In the literature, for maximum ET, there is no consensus on a cutoff value for a normal endometrial echo in postmenopause for either symptomatic or asymptomatic women. In fact, through the years, different ET-cutoff values have been proposed as a reliable, noninvasive approach to rule out EC in patients with PMB.
- From 57 studies with 9031 patients, the commonest ET cutoffs were 4 mm and 5 mm, but only four studies were identified as being of best quality. Pooling of the results of these four studies for ET 5 mm or less resulted in a likelihood ratio of a negative test of 0.16. Such a likelihood ratio would imply that in a patient with a negative test result, a pretest probability of 10% would change to a posttest probability of 2.5%. As such, the authors concluded that ET ?5 mm detected by ultrasonography can be used to rule out endometrial hyperplasia or carcinoma with good accuracy.
- In current practice, many postmenopausal women without symptoms undergo TVUS as part of a routine gynaecological checkup, eg, to investigate abdominal pain or masses, delineate the adnexa when pelvic examination is inadequate, or evaluate a uterus prolapse, but usually TVUS without indication is not recommended. As such, an incidental finding of endometrial thickening in postmenopausal women without vaginal bleeding represents a clinical management dilemma, because there is a lack of consensus among gynaecologists.
Symptoms of Thickened Endometrium
Endometrial hyperplasia may be asymptomatic or lead to several symptoms, such as vaginal discharge, bleeding between menstrual cycles, heavy and/or prolonged menstrual bleeding, and pelvic and/or abdominal pain.
Diagnosis and Treatment for Thickened Endometrium
Diagnosis of thickened endometrium can be easily confirmed with the assistance of an ultrasound of the uterus. What follows is a biopsy of the endometrium and a pathohistological examination of the biopted tissue so that the underlying cause can be properly identified.
Treatment for thickened endometrium depends on the underlying cause and may be conservative or surgical. Most of the time simplex or complex hypertrophic endometrium without cellular atypical is treated with birth control pills or progesterone.
Women who are in menopause, particularly those suffering from atypical endometrial hyperplasia are perfect candidates for hysterectomy, a surgical removal of the uterus. This is both, the treatment for endometrial hyperplasia and the method of prevention against potential endometrial cancer.
- www.nhs.uk/conditions/womb-cancer/
- medlineplus.gov/ency/article/000910.htm
- Photo courtesy of Nephron by Wikimedia Commons: commons.wikimedia.org/wiki/File:Endometrium_ocp_use0.jpg

















Your thoughts on this
Loading...