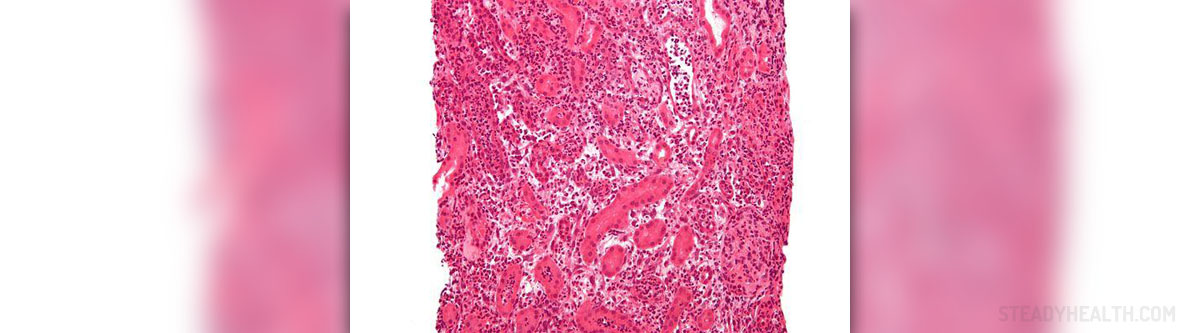
Lymphatic obstruction, damage of the alveolar-capillary barrier and certain imbalance of Starling forces may cause pulmonary edema. This condition happens when the fluid start leaking from the pulmonary capillaries into the lungs and alveoli.
Recognize the Symptoms
Acute pulmonary edema is medical emergency and it should be treated as such. Patients may be severely lacking the breath, feel nauseous, anxious and sweaty. Paroxysmal nocturnal dyspnea or orthopnea and some dry cough are often seen in these people. Pale skin, sweat, tachycardia and tachypnea, congested neck veins and raised JVP could also indicate pulmonary edema.
Besides these signs, patients may also experience lack of oxygen saturation, 3rd heart sound and murmurs, hypotension, oliguria and other symptoms depending on the cause of this problem.
Causes of Pulmonary Edema
Raised pulmonary capillary pressure, increased permeability or pulmonary capillaries, lymphatic obstruction and obstruction of upper airways (either acute or chronic) can lead to development of pulmonary edema. This includes medical conditions of the heart and lungs, as well as various other health issues, which all have been known to cause this problem.
When it comes to heart related problems that might provoke acute pulmonary edema, ischemic heart diseases such as myocardial infarction or acute coronary syndromes are often found to be the cause of this problem. Acute aortic or mitral regurgitation, endocarditis and severe aortic stenosis may also cause the same condition. Acute myocarditis, acute arrhythmia, aortic dissection and cardiac tamponade can also lead to pulmonary edema. Left atrial myxoma, cardiomyopathy and the use of drugs known to cause myocardial depression or fluid retention are also possible explanation for pulmonary edema.
Renal artery stenosis and renal failure (whether acute or chronic) could also cause the same problem.
High output heart failure, seen in anemias, shunts, thyrotoxic crisis or septicemia, as well as iatrogenic fluid overload and cerebrovascular insult may lead to acute pulmonary edema as well.
People in high altitudes or those suffering from acute respiratory distress syndrome (also known as ARDS), liver failure, fat embolism or amniotic fluid embolism can also experience acute pulmonary edema. Additional explanations for this problem include: inhalation or aspiration of certain toxic substances, radiation or obstruction of the airways. In some cases, lymphatic obstruction, due to silicosis or mediastinal carcinomatosis is also associated with pulmonary edema.
Diagnosis and Management of Acute Pulmonary Edema
This condition requires urgent stabilization and investigation. Doctors may require blood tests, ECG, echocardiogram (ESC), chest X-ray, urinary catheter and some non-invasive and/or invasive monitoring of the patient.
Treatment involves improvement of oxygenation, perfusion and hemodynamics and prevention of potential further damage to the heart and the kidneys. Emergency ambulance, resuscitation, oxygen when available and hospitalization are possible options. In the hospital, patients may be sedated, given some pain killers, nitrates or furosemide.















Your thoughts on this
Loading...