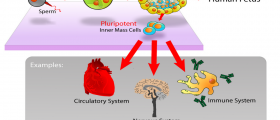
There are many types of cancer. One of the best treatments for cancers is the bone marrow transplantation. This procedure can be extremely painful but can also give great results. This treatment is also called stem cell transplantation. The full array of cancers can be affected by the process.
Such are malignant myeloma, leukemia, aplastic anemia, non Hodgkins lymphoma and many other. The recovery from this procedure can sometimes be very long and tiring. So we will try to explain what awaits the patients after the bone marrow procedure.
Bone Marrow Transplant Procedure Step by Step
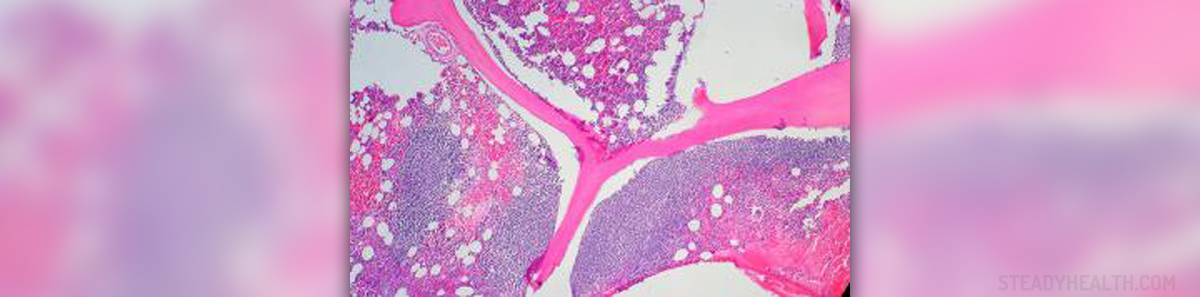
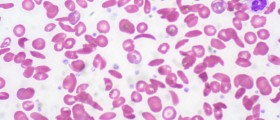
The process of bone marrow starts with the elimination of the complete bone marrow from the patient's body. This is done by radiation and chemotherapy. After this, the harvested stem cells are returned back to the patient. This part of the process is named autologous transplantation.Nowadays, doctors try to use as less as chemotherapy and radiation as possible, since they can cause serious discomfort to the patients. But this is only done with patients which are in stronger condition, because some side effects are possible. They do not destroy all the bone marrow and leave just a small portion of it.
The chemotherapy has many side effects and one of the most serious is the weakening of the immune system. The immune system is even nonexistent in the first 2-4 weeks after the cell transplant. Because of this, it is important to be in sterile conditions until the stem cells recover.
Until this happens, patients are located in rooms with filtered air, cannot be visited by friends and family and will have very limited diet. Patients will have long recovery. Even when they are dismissed from the hospital, they must remain in their homes for the next several months. They cannot return to work before six months and in some cases even a year.
- We know from population-based studies that only 20% to 25% of patients eligible for allogeneic transplantation will have suitable sibling donors.
- To make transplantations available to a greater number of eligible patients, registries of volunteer bone marrow donors have been developed. These can provide transplant physicians with stem cells from unrelated but matched donors. More than 6 million donors are registered on national donor panels worldwide.
- Cord blood from neonates contains substantial numbers of hemopoietic stem cells, which can be harvested at delivery, frozen, and then transplanted to patients who would not otherwise have a donor. Thousands of such donations are now stored in special banks worldwide, after cell counts and virologic screening tests are performed, and inventories of their HLA types are available to transplantation centers. Computer records can be scanned quickly, and donations can be matched with possible recipients without the delays inherent in securing an adult donor. The first cord blood transplantation was performed in 1989 by Gluckman and Broxmeyer, and since then more than 700 successful transplantations have been made.
- Autologous transplantation (patients are their own donors) is now the most common form of stem cell transplantation. Cryopreservation techniques now allow bone marrow to be stored safely and indefinitely, while the patient undergoes conditioning chemotherapy, without catastrophic loss of stem cells on thawing. Recovery of peripheral blood cell counts after cryopreserved marrow previously exposed to chemotherapy was transplanted was slow, and patients had prolonged neutropenia and thrombocytopenia. However, no graft-versus-host disease or prolonged immunosuppression developed, and the procedure was safer than with allogeneic transplants.
- Stem cell transplantation is associated with substantial morbidity and (in allogeneic transplantation) mortality. Patients may spend considerable time in the hospital and need prolonged convalescence, especially if they are affected by graft-versus-host disease. However, several advances are associated with an improved outlook for patients and have led to increased interest in stem cell transplantation as a treatment.
- The most important factor affecting the outcome of allogeneic transplantation is the quality of the HLA match between donor and recipient. New DNA-based techniques allow more sophisticated matching and are improving the outcome of this type of transplantation, particularly for unrelated transplants.
Graft Versus Host Disease
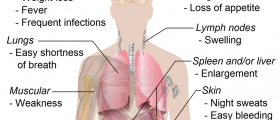
There is a possibility of the development of a condition called graft versus host disease. The symptoms will not develop before three months after the surgery. This disease is lethal in every fifth or tenth case, and causes skin rash, nausea, kidney and lung problems, vomiting, dry eyes and jaundice.But the consolation for the people with this condition can be found in the fact that they remain cancer free usually longer than the patients which never develop the disease. The patients who take donor cells usually develop the condition, while the one's who use a mix of donor and patient's cells always do. Process with the patient's cells never produces the graft versus host disease.
There is also the possibility of developing the acute disease which can last for 18 months. Although the treatment is long, painful and dangerous, the results may be worth the effort. Know that there are many support groups and doctors which will help you recover from the bone marrow transplantation.











Your thoughts on this
Loading...