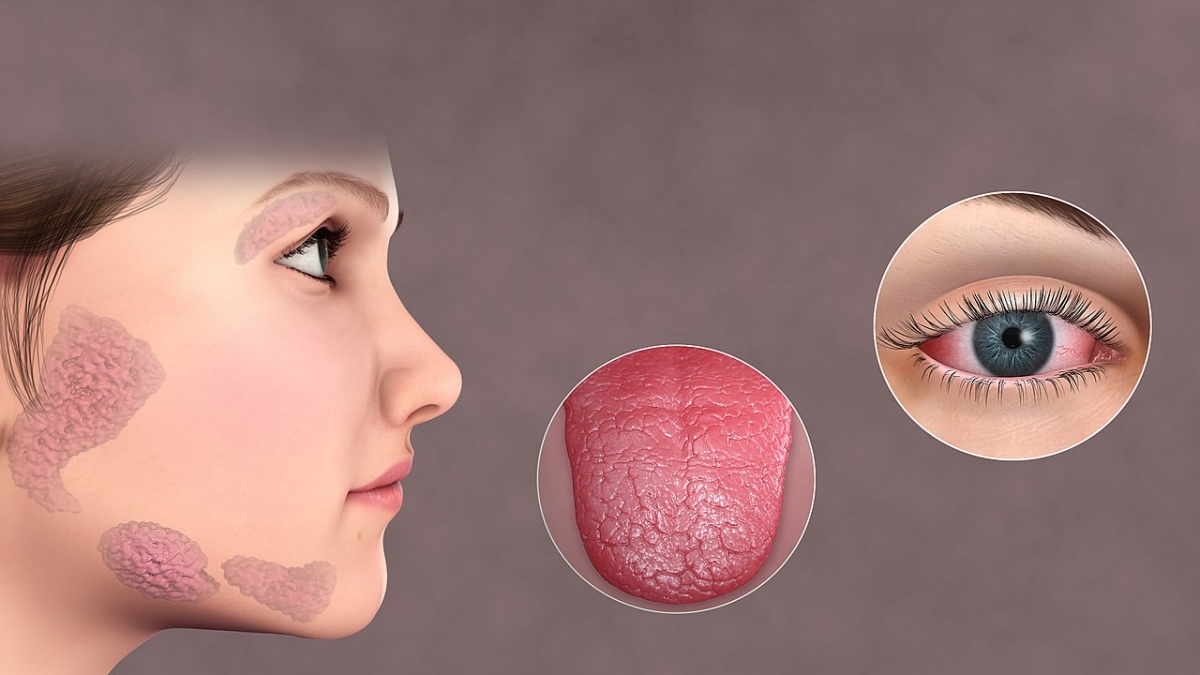
Sjogren's syndrome is a member of the autoimmune group of diseases. This medical condition is characterized by an inflammation of various glands and other tissues of the body and predominantly affects women. The inflammation and subsequent damage as well as complications of the disease are all closely related to the presence of antibodies against a variety of body tissues.
The diagnosis of Sjogren's syndrome is established thanks to clinical manifestations as well as a detection of antibodies in the blood and a biopsy of certain tissues (the saliva gland in particular). As for treatment, Sjogren's syndrome is basically managed by dealing with the symptoms of the disease along with complications.
When it comes to neurological complications of the disease they are classified into several groups including neuromuscular manifestations, CNS complications and finally, subclinical disease.
Neuromuscular Manifestations of Sjogren's syndrome
Patients suffering from Sjogren's syndrome may develop a whole variety of neuromuscular complications. Let us begin with myalgia. This is an inflammation of muscle tissue accompanied by spontaneous pain or pain induced by palpation (simply said, touching). Patients affected usually report difficulty climbing stairs because of the accompanying muscle weakness. Inflammation of muscle tissue may also be completely asymptomatic. The disease tends to progress over time and even cause muscle fiber necrosis which is confirmed with an elevated sedimentation rate and muscle enzymes, electromyography as well as muscle biopsy.
Furthermore, patients may additionally develop neuropathy of different kinds. This condition is characterized by paresthesia, an abnormal sensation occurring in the form of tingling, burning, pricking, or numbness of a person's skin with no obvious long-term physical effect. Neuropathies associated with Sjogren's syndrome predominantly affect the legs.
Depending on whether the neuropathy affects sensorineural or motor neuron patients develop different symptoms. If many nerves in the body get inflamed and damaged, the condition is known under the name multiple mononeuropathy. Polyradiculoneuropathy is characterized by the inflammation of various nerves and nerve roots and is actually the most severe form of the disease.
In the end, one more type of neuropathy which patients suffering from Sjogren's syndrome may eventually develop is trigeminal neuropathy. It is a cause of progressive sensory complaints on the face which is in the beginning unilateral and after some time may affect the other trigeminal nerve.
Central Nervous System Complications of Sjogren's syndrome
In rare instances, patients living with Sjogren's syndrome additionally develop abnormalities within the central nervous system. There may be changes affecting solely the brain or the spinal cord, or both organs get damaged.
Focal deficit disorders are typical for this form of the disease. They may precipitate motor or sensory loss along with hemiparesis (weakness on one side of the body), aphasia (a language disorder), dysarthria (a motor speech disorder) and movement disorders. Seizures and cerebellar syndrome may occur as well.
Diffuse disorders develop in the form of encephalopathy and aseptic meningitis, dementia, impaired cognitive function or even psychiatric abnormalities.
When the spinal cord gets damaged, patients with Sjogren's syndrome may develop transverse or chronic progressive myelitis. They are also susceptible to neurogenic bladder or end up with Brown-Séquard syndrome or lower motor neuron disease.
Psychological and behavioral changes that might occur along with the basic symptoms and signs of Sjogren's syndrome include a lack of concentration and attention, a subcortical dementia, hysteria, hypochondriasis, depression, dysphoria and sometimes anxiety or panic attacks.
Subclinical Disease and Differential Diagnosis
Because of its clinical manifestations, Sjogren's syndrome may be easily confused with other autoimmune diseases. For instance, Sjogren's syndrome is sometimes mistaken for multiple sclerosis when a patient first seeks medical attention and diagnosis. The aforementioned neurological manifestations of Sjogren's syndrome are also reported in the majority of patients suffering from multiple sclerosis. This is the reason why the two disorders often look alike. However, the presence of peripheral nervous system disease would help doctors exclude multiple sclerosis as a potential diagnosis in these patients.
Furthermore, there is a resemblance between systemic lupus erythematosus and central nervous system involvement in patients with Sjogren's syndrome. This particularly refers to multifocal neurological deficits and manifestations. Still, there is a slight difference. Namely, in systemic lupus erythematosus seizures occur more commonly compared to Sjogren's syndrome. On the other hand, Sjogren's syndrome is much more a reason why patients eventually end up with focal deficits. The hardest task would be the differentiation of the two conditions if concentration and cognitive disorder are present or there are vasculopathies/microinfarction of the brain/spinal cord, since all of these occur almost equally in case of SLE and Sjogren's syndrome.
All in all, there is a whole variety of neurological complications affecting individuals with Sjogren's syndrome and these must be differentiated from neurological diseases like Parkinson’s disease (a movement disorder, with some symptom similarities with Sjogren's syndrome), Guillain Barré syndrome, or Alzheimer's multi-infarct dementia along with the already mentioned multiple sclerosis. Only after the condition is confirmed can doctors opt for the most suitable treatment.
The goal of the treatment patients with Sjogren's syndrome receive is to reduce inflammation and the accompanying neurological issues which can be achieved with several types of medications including corticosteroids, immunosuppressive agents such as azathioprine, chemotherapeutics such as cyclophosphamide and in the most severe cases IVIG.
In the end, neurological manifestations of the disease should be detected and confirmed as soon as possible and treated aggressively. By doing so, long-term complications of Sjogren's syndrome would be minized, and the treatment would be much more successful.
- www.nhs.uk/conditions/sjogrens-syndrome/complications/
- www.nhs.uk/conditions/sjogrens-syndrome/
- Photo courtesy of Scientific Animations via Wikimedia Commons: commons.wikimedia.org/wiki/File:Sjogrens_Syndrome.jpg













Your thoughts on this
Loading...