
Post-polio syndrome (PPS) is the term used for a set of symptoms and signs all of which occur many years after the initial polio illness. In the majority of cases the syndrome occurs decades after the the initial disease (after 15-30 years). Polio (poliomyelitis) is a severe viral infection associated with permanent neurological sequelae among which partial or full paralysis are the two most severe ones. Fortunately, the disease is today rare since there is obligatory vaccine against the virus.
PPS Comes after Surviving Polio
There are many theories which try to explain why post-polio syndrome occurs. However, there are no conclusive evidence regarding the onset of post-polio syndrome or identified causes of why some symptoms and signs occur after so many years. Out of all theories scientist seem to accept one the most. It says that post-polio syndrome develops as a consequence of 'neural fatigue'.
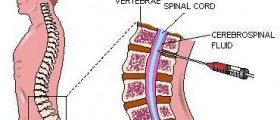
Namely, anatomically a motor unit comprises a nerve cell and the muscle fiber the particular nerve innervates. Now, the virus attacks and causes damage to neurons localized in the brainstem and certain parts of the spinal cord. This leads to death of many motor neurons which are in charge of control of skeletal muscles. In order to repair damage to some extent surviving motor neurons develop new nerve terminals and send these to the affected nerves. By doing so they restore movement to certain degree.
The neural fatigue theory is actually based on the previously assumed course of the disease. It appears that there is excessive metabolic stress placed on the nerve that need to nourish their own fibers and additional muscle fibers, the ones that lost their nerve supply during the initial disease. The stress is blamed for lack of sufficient nourishment of all fibers and this leads to their gradual deterioration (weakness and paralysis). Even though some function can be restored for the second time, weakness due to permanent malfunction inevitable occurs.
The process of aging also needs to be taken into consideration because it is a well known fact that when we age the number of spinal motor neurons decreases. So, in patients who had polio such reduction is more obvious because they already developed certain degree of motor neuron dysfunction.
As far as symptoms and signs of post-polio syndrome are concerned, these include progressive muscle weakness, unusual fatigue, and muscle atrophy. It is also possible for one to experience pain due to joint degeneration and associated skeletal deformities. Scoliosis is, for example, only one deformity these patients are prone to.
Doctors confirm the syndrome by using specific criteria. Firstly, they need to confirm acute paralytic illness, the presence of residual weakness and muscle atrophy while performing neuromuscular examination and with the assistance of EMG (electromyography). The period of complete functional recovery after initial polio disease needs is also important. What is more, there need to be gradual or rapid onset and progression of new neurological signs like muscle weakness, atrophy and fatigue. These symptoms must last at least for a year and it is of major importance to exclude other potential neuromuscular or similar medical conditions.Is PPS Life Threatening?
Fortunately, in the majority of cases post-polio syndrome is not life-threatening. Only if weakness affects the respiratory muscles one may have severe shortness of breath which sometimes leads to lethal outcome. Similarly, weakness of swallowing muscles may lead to food aspiration.
The severity of the initial disease seems to play an important role in the severity of post-polio syndrome symptoms and signs. Namely, patients who did not have complex neurological issues and only dealt with mild form of the initial disease usually develop mild symptoms of post-polio syndrome. On the other hand, those who faced more complex symptoms and signs of the initial disease develop severe form of post-polio syndrome with uncertain outcome.
Treatment for post-polio syndrome is basically palliative. It comprises plenty of rest, analgesia (if necessary) and some assistive devices which will allow patients to function better on their own, not being dependent on other people (relatives or caregivers).
There is no available treatment that can reverse progression of muscle weakness and accompanied muscle atrophy. Still, there are some changes in lifestyle which can be of great assistance. For instance, energy conservation may drastically reduce fatigue episodes. One should also reduce workload and make dietary changes in order to achieve healthy weight. Some doctors try to deal with fatigue by prescribing certain drugs (e.g. amantadien or pyridostigmine) although these have not been confirmed to successfully reduce fatigue. Additional help can be achieved with muscle strength and endurance training.
One of common health issues these patients face with are difficulty eating and malnourishment. Also, the muscles involved in the process of breathing may be too weak. But even these patients may continue living their lives as normally as it is possible with additional treatment and support.














Your thoughts on this
Loading...