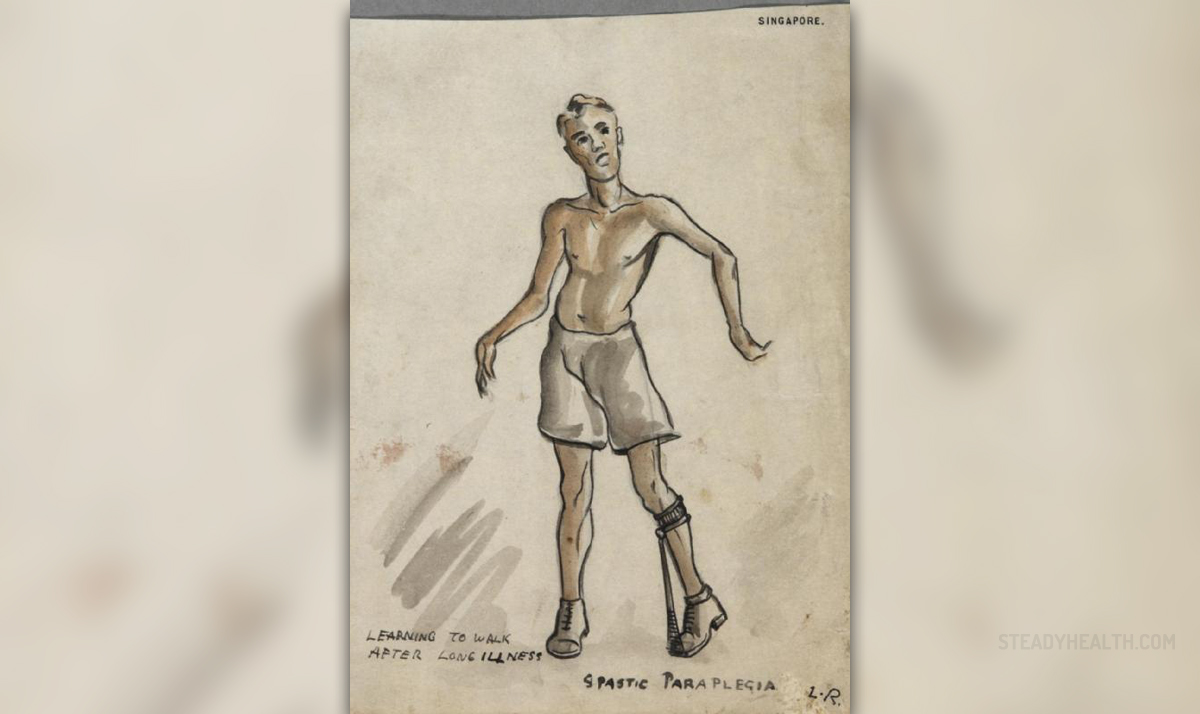
Familial spastic paraplegia syndrome, also known under the name hereditary spastic paraplegia, represents a group of rare medical conditions characterized by spasticity in the lower extremities. The spasticity is progressive, develops as a result of damage to nerve tissue and may be rather severe in nature.
Apart from typically affecting the nerves innervating the lower extremities, in some cases the syndrome is additionally associated with several more health issues including damage to the optic nerve, cataract, ataxia, seizures, peripheral neuropathy and hearing loss. Cognitive impairment may occur as well.
Hereditary Spastic Paraplegia
The syndrome develops due to defects regarding mechanisms important for adequate cellular transfer of different substances.
As far as pathohistological changes are concerned, the leading damage affects axons. Namely, there is axonal degeneration. Such damage is most extensive in the terminal parts of the longest descending as well as ascending tracts. Other tracts such as the spinocerebellar tract may not be affected at all or they suffer less damage. The process of demyelination does not occur.
This group of illnesses is classified according to symptoms and signs patients develop and the mode of inheritance. The age of the patient when the first symptoms occur is also taken into consideration.
Pure hereditary spastic paraplegia is only a cause of spasticity while there are no associated health issues. Complex hereditary spastic paraplegia, on the other hand, is characterized by the presence of several more conditions some of which are dementia, epilepsy and mental retardation. These patients may have other neurological signs as well.
When it comes to mode of inheritance, the syndrome may be inherited in practically all ways including an autosomal dominant fashion, autosomal recessive fashion, mitochondrial and X-linked recessive inheritance.
In the majority of cases patients inherit the disease in an autosomal dominant fashion. In this case, one of the parents, either the mother or the father passes the gene to their child. One gene is sufficient enough for the child to develop the syndrome. In case of an autosomal recessive inheritance, both parents must have the defective gene and the child develops the syndrome only if both copies of the gene are passed. The inheritance related to X chromosome is a bit different. Namely, women are known to have two X chromosomes while men have only one. This explains why symptoms and signs of hereditary spastic paraplegia are much more severe in men that inherit the condition in such a way. Women may have one normal X chromosome and develop symptoms or remain carriers.
And finally, classification based on the age of the disease onset includes two types of the disease. In type 1 patients are younger than 35 while those suffering from type 2 of the disease are older than 35. What is more, Type 1 of hereditary spastic paraplegia patients face severe spasticity and moderate weakness in the lower extremities while patients with type 2 of the disease have to deal with more intense weakness, severe sensory loss and are prone to urinary issues. The progression is also more rapid in case of type 2 hereditary spastic paraplegia.Management of Familial Spastic Paraplegia
There is no efficient treatment that may cure hereditary spastic paraplegia. However, symptoms and signs of the disease may be brought under control with symptomatic treatment. There are medications which reduce spasticity and beneficial effects are additionally achieved with physical therapy. Such patients also require assistive devices and communicational aids, support from their family, friends and co-workers.
Physical therapy is an excellent means of maintaining muscle strength. It also improves the range of motion and reduces the spasticity. The process of degeneration will continue in spite of this treatment modality. Still, the effects such as an increase in muscle strength, reduction of fatigue, prevention of spasms and muscle atrophy can be satisfying enough for one to continue exercising. Patients must stick to their exercise program and remain active several times per week. Apart from physical benefits, exercise also reduces, if not completely eliminates the stress from the patient's life. The exercise program must incorporate several types of exercises including strengthening exercises, stretching exercises and aerobic exercises.
Despite the huge effort to reduce the risk of complications, patients many times develop additional health issues which require other treatments as well. Most common complications associated with hereditary spastic paraplegia are contractures (e.g. gastrocnemius-soleus contracture), problems with circulation (cold feet), extreme fatigue and pain affecting the back or the knee. These patients are also prone to depression.
All in all, hereditary spastic paraplegia is a progressive disease inevitably leading to bed confinement. Fortunately, the prognosis is different and many patients with proper supportive care and physical therapy may remain active for a long period of time or reduce the extent of disability significantly. Even those in whom the disease has progressed may have productive and full lives thanks to a variety of modern assistive devices.















Your thoughts on this
Loading...