Hemispherectomy is an invasive surgical procedure during which the surgeon removes the entire half of the brain. This is not routine surgery. In fact, hemispherectomy is only indicated in patients suffering from severe forms of epilepsy in whom the abnormal electrical activity remains localized onto one cerebral hemisphere and whose symptoms simply cannot be well controlled with any of the available antiepileptic agents.
Removal of Part of the Brain
The first such procedure was performed on a dog in 1888 while the first hemispherectomy done in humans took place in 1923 on a patient suffering from glioblastoma multiforme, a highly malignant type of a brain tumor. During the 1960s and 1970s the procedure was further investigated but because of certain side effects doctors were not so sure whether it is efficient or only triggers certain side effects. Namely, the major problem was the filling of the empty space in the cranium with excess of fluid and the accompanying increase in intracranial pressure and subsequent compression of the remnant of the brain. Fortunately, hemispherectomy was reborn in 1980s. The surgery was a bit modified while its raw essence (the pure, traditional 'anatomic' hemispherectomy) remained a powerful tool reserved only for people wit severe forms of epilepsy.
Functional hemispherectomy is a modified type of traditional hemispherectomy and widely acceptable treatment approach. The surgery includes removal of specific portions of one hemisphere, basically those which are used the least. The surgery additionally includes cutting of the corpus callosum, the part of the brain that connects the right brain hemisphere to the left one. By cutting the connection between the two hemispheres further transmission of abnormal electrical impulses is practically discontinued.
When we discuss potential candidates for functional hemispherectomy, individuals with no response to conventional treatments and a wide variety of antiepileptic agents are definitely worth of mentioning. Namely, these patients do their best and take prescribed medications but still face frequent epileptic attacks. The attacks interfere in their everyday activates, make them incapable of performing some duties or even get a job and also might have detrimental or irreversible effects on certain brain functions. The epilepsy with all the mentioned characteristics is mostly reported in children who are suffering from Rasmussen's encephalitis or Sturge-Weber syndrome but it affects older persons as well.
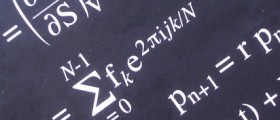
Prior to function hemispherectomy all candidates undergo a thorough pre-surgery evaluation. Their seizures are monitored and recorded, they undergo electroencephalography and MRI of the brain. The tests assist in confirmation of the damage to the affected half of the brain and also identify the source of the epileptic attacks. It is also essential to perform an intracarotid amobarbital test (WADA test) which establishes which brain hemisphere is dominant for certain functions.
The very procedure takes place in an operating room, under general anesthesia. A team of neurosurgeons is included. The head is opened (doctors perform craniotomy) which allows better insight in the organ and makes the resection and removal easier. After making a hole in the skull, surgeons remove the superficial membranes of the brain and eventually reach the very surface of the organ. Hemispherectomy requires surgical microscopes. These provide with a magnified view of the brain structures. In the majority of cases the entire temporal lobe is removed along with other portions of the affected hemisphere. Some parts of the brain remain intact such as frontal and parietal lobes. Surgeons additionally make a cut in the corpus callosum this way separating the right brain hemisphere from the left and discontinuing the transfer of electrical impulses.
After the surgery patients are transferred to the intensive care unit where they spend about 24-48 hours and then remain hospitalized for additional 3-4 days. The recovery lasts between 6 and 8 weeks. After this period of time most people return to their work and children to school. Even though the source of the epileptic attacks is removed, patients may need to continue taking antiepileptic drugs. The dose of these drugs is, however, reduced.
How Effective is Functional Hemispherectomy?
According to available data 85% of all operated individuals will experience considerable improvement in their seizures. What is more, 60% of them will become seizure-free, reaching the goal of the surgery. The preserved brain hemispheres will take over the tasks and functions of the removed portions of the brain. This is observed in children, while it might not be fully achieved in older individuals. All in all, the quality of patient's life significantly improves.
Still, there are potential side effects of the procedure that may leave a permanent trace on the patient's life. Apart from general side effects that are transient and easily managed there are far more complex issues like swelling of the brain, loss of movement/sensation on the opposite side of the body, loss of peripheral vision, delayed development and damage to the remnant hemisphere.
This is why hemispherectomy is almost exclusively performed in children in whom the neurons from the preserved portion of the brain may easily take over the tasks of the removed parts and by doing so restore all the functions that would be otherwise lost.




_f_280x120.jpg)








Your thoughts on this
Loading...