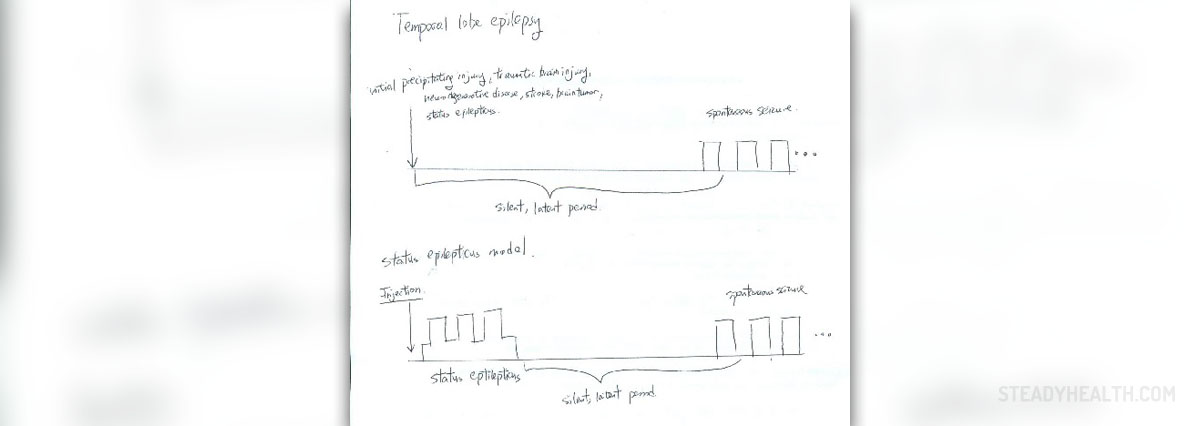
Temporal lobe epilepsy is the term that refers to seizures originating from the temporal lobe of the brain. The temporal lobe is normally in charge of processing emotions and is also engaged in fight-or -flight reactions. This part of the brain is essential for short-term memory. Now, once electrical activity in this part of the brain becomes abnormal, one develops epilepsy. Abnormal electrical discharge may affect only neurons in the temporal lobe or spread to the entire brain precipitating generalized seizures.
Complications of Temporal Lobe Epilepsy
The underlying cause of this type of epilepsy is in the majority of patients unknown. Scars or anatomical defects may, however, be reasons behind temporal lobe epilepsy.
Patients suffering from this type of seizures may experience a so called aura before the attack. This is an introduction to actual seizures most commonly characterized by a sudden onset of unusual fear, déjà vu sensation, unexplained occurrence of a strange odor or taste or even a rising sensation in the stomach. Auras are actually very helpful because they warn patients about the forthcoming attack so they can get prepared.
The very attack is associated with complete loss of consciousness when patients cannot recall anything that happened or they remain conscious to a certain extent. The attack usually does not linger more than 2 minutes. It is typically accompanied by staring, lip smacking, repeated swallowing or chewing and atypical finger movements (e.g. picking motions). Most patients find it hard to speak immediately after the attack or experience mild confusion. It is also possible that they do not realize they have just had seizures until they are explained what has happened. Rarely, localized seizures initially affecting the temporal lobe spread to other parts of the brain and trigger generalized seizures associated with convulsions and complete loss of consciousness.
As far as complications of the condition are concerned, these may be rather severe and cause irreversible damage to the temporal lobe, hence interfere with functions this part of the brain is in charge of. First of all, seizures make patients susceptible to injuries especially if there is loss of consciousness during the attack. Such patients are, therefore, prone to fractures, tongue lacerations, dental injuries, shoulder dislocation etc. Furthermore, they are at risk of aspiration pneumonia, Mallory-Weiss tear and may eventually develop depression. Learning disabilities and memory problems may occur as well. Patients who are heavily medicated develop many antiepileptic side effects. Adverse effects of these medications are also possible if low doses are administered for a long period of time. Finally, in patients prone to status epilepticus seizures last more than 30 minutes, they are multiple and may be connected with rhambdomyolysis.
Surgery can be a Solution
Since temporal lobe epilepsy may be easily resistant to antiepileptic medications such patients are practically left with only one treatment option - surgery. This is a complex surgery always performed by a well-experienced neurosurgeons. There are risks associated with the procedure. However, they do not have to occur and can be successfully avoided and patients provided desirable results. Prior to the surgery, doctors evaluate patients and determine whether they are suitable candidates for the surgery and if there are any contraindications. Normally, it is essential to perform specific tests and exams that will confirm that seizures actually originate from the temporal lobe and not other parts of the brain. This is achieved with EEG (electroencephalography).
Temporal lobe resection, also known as temporal lobectomy, is a complex surgical procedure and a type of epilepsy surgery. During the procedure the temporal lobe, the focus of epileptic seizures, is surgically removed. Once the very focus of the attack is localized a surgeon removes the affected part i.e. performs a resection of this part of the temporal lobe. It is amazing how seizures can drastically reduce after the procedure. In some patients epileptic attacks are practically completely eliminated. It is essential not to damage vital centers in the temporal lobe, the ones in charge of memory, language and emotions.
As it is the case with practically every surgery even temporal lobe resection carries a certain risk and may be connected with several complications. The most commonly reported problem after the surgery is loss of peripheral vision. It affects around 25% of operated individuals. Furthermore, there may be speech and languages issues. Such problems affect 10% of patients. Fortunately, the majority of patients eventually restore lost functions completely. Permanent problems with memory are infrequent thanks to tests performed prior to and during the very procedure. Finally, even though lethal outcome is practically impossible, 0.1% of operated patients may die during the surgery. This complication is basically associated with some already existing conditions.
When it comes to results, 70% of operated individuals still have seizures but they remain conscious during the attack and there are no convulsions present. It is also possible for patients to experience an aura but still do not develop seizures. Approximately 20% of patients will continue having seizures after the operation. The symptoms and frequency of the attacks, however, are reduced. And finally, 10-15% will experience no improvement even after being operated. Future treatment of this group of patients can be rather challenging and demanding.













Your thoughts on this
Loading...