The prostate gland is a conical-shaped organ the size of a walnut. It is part of the male reproductive system. The prostate gland is located in front of the rectum and just below the bladder. It surrounds the urethra, which is the tube that carries urine from the bladder to the penis.
The prostate gland is made out of 30% of muscular tissue and 70% of glandular tissue. The size of the prostate gland remains the same until puberty when it doubles in size. It gradually grows after the age of about 50, and in some men, this enlargement can cause bothersome symptoms.
Prostate Gland Function
The prostate gland requires hormone testosterone to function properly. Testosterone helps the gland regulate bladder control and normal sexual functioning. The main function of the prostate gland is to secrete and store seminal fluid. This fluid is milky or white and contains several enzymes, citric acid, and calcium that nourish the sperm cells.
During ejaculation, this fluid is added to semen. It is alkaline and protects the semen by neutralizing the acidic environment of the vagina. This way, it prolongs the lifespan of sperm and promotes sperm motility. This means that the prostate gland actually helps to increase the chance of impregnation.
Another function that the prostate gland performs is to seal off the urethra during the ejaculatory process. This prevents urine from entering the urethra and urination during sexual intercourse. This function of the prostate gland can be impaired in some men over 50 years. This can be seen in men with enlarged prostate, which can constantly constrict the urethra and impede the flow of urine even when an affected individual does not engage in sexual activity of any sort.
The prostate gland also aids in the liquefaction of semen after ejaculation. This is due to an enzyme called a prostate-specific antigen (PSA) that the cell lining the prostate secretes into the seminal fluid.
- The prostate gland idivides anantomically into five lobes: anterior and posterior lobes, two lateral lobes, and one median lobe. This description is in many anatomical textbooks. In clinics, it is described as having two lateral lobes right and left and a median lobe.
- Importantly, the prostate gland has multiple tubular structures passing within it, including the proximal urethra and two ejaculatory ducts. The ejaculatory ducts enter the prostate immediately as it emerges from the seminal vesicles. Both of these ducts travel from posterior and lateral to medial and inferior. They ultimately converge at the urethra within the prostate gland on an area called the seminal colliculus.
- The prostate gland starts to develop laterally as epithelial buds from the urogenital sinus wall. These buds branch into solid cords which canalize and form the ducts and acini. The surrounding urogenital sinus mesenchyme forms the interfascicular fibroblasts and the smooth muscle of the prostate. With androgenic stimulation of the androgen receptor expressed in prostatic Mullerian mesenchyma, the prostate forms. In development, androgen secretion by Leydig cells is the chief regulator of prostate growth.
- As the prostate gland shares a close anatomical relationship with the bladder, it also shares a portion of the bladder’s blood supply. The inferior vesical artery is the major blood supply for the prostate, and it also receives blood supply from the middle rectal and internal pudendal arteries.
- The prostate gland receives innervation via the autonomic fibers from the inferior hypogastric plexus, receiving sympathetic input from the hypogastric nerve. Parasympathetic inputs derive via the pelvic nerve. Both the hypogastric and pelvic plexuses provide sensory inputs for the prostate.
Prostate Disorders
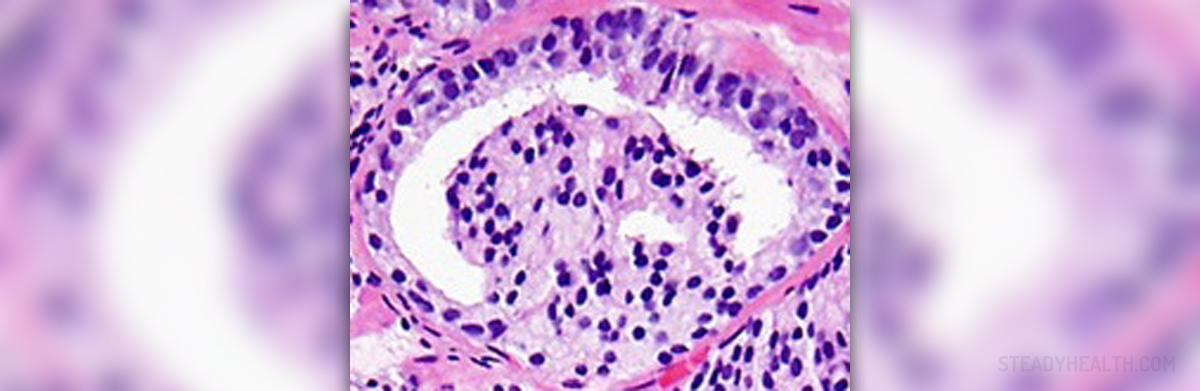
The prostate gland can be affected by several disorders. Prostatitis is an inflammation of the prostate gland caused by bacterial infection. There are four different forms of prostatitis. An enlarged prostate, also known as benign prostatic hyperplasia (BPH), is a non-cancerous growth of the prostate which causes difficulty in urinating.
Common symptoms of an enlarged prostate are frequent need to urinate, urinary incontinence, and weak urine stream. This condition usually affects men aged over 60. Prostate cancer is a life-threatening disease that affects a significant percentage of the male population in developed countries. It is one of the most common cancers in older men.
Prostate cancer grows slowly and usually does not spread for many years. Symptoms of prostate cancer include difficulty in urinating, pain during urination, appetite loss, weight loss, painful ejaculation, and blood in urine.
- www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/prostate-gland-and-urinary-problems
- medlineplus.gov/ency/article/004017.htm
- Photo courtesy of Jennifer Gordetsky and Jonathan Epstein by Wikimedia Commons: commons.wikimedia.org/wiki/File:Micrograph_of_prostate_adenocarcinoma_with_a_glomeruloid_gland.jpg
















Your thoughts on this
Loading...