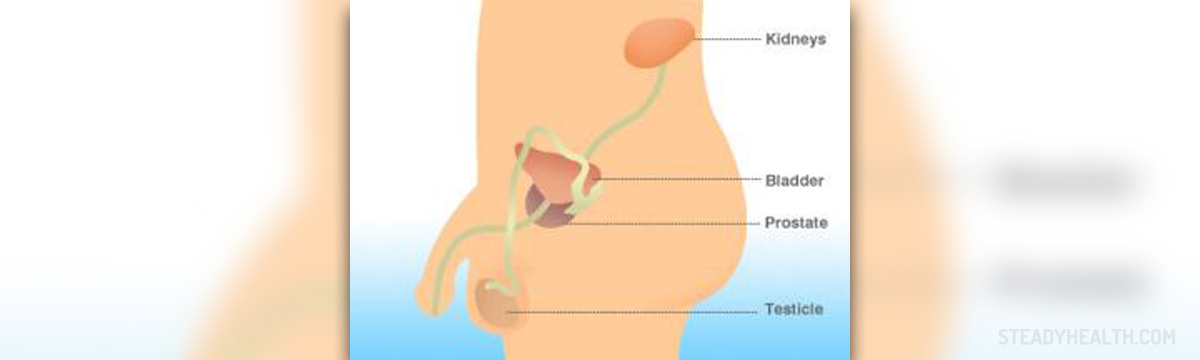
Prostate Definition
The prostate is male reproductive gland that is responsible for producing the fluid that carries sperm in times during ejaculation. Surrounding urethra, trough witch urine passes out of the body, in same cases gland grows bigger, pressing it, and causing bladder and urination problems. This state is called Prostate enlargement or Benign prostatic hyperplasia - BPH, and happens to almost all men in their older age. Half of men will experience prostatitis (infection) of prostate even once in their lifetime.
Infection that can cause prostate swelling is defined in 4 categories;-chronic abacterial prostatitis-chronic bacterial prostatitis-Prostatodinya (prostate gland pain)-acute bacterial prostatitis
Of this four, causes are known only for chronic and acute bacterial prostatitis is known. For rest, causes remain unknown.
Causes of Prostate Infection
Real causes are unknown for 95% of cases, but only 5% of infection cases are explained. Infection has two ways of spreading. First is when bacteria from older urinary infection moves to attack prostate. Second is the case when infected urine is moving through prostatic ducts. There is also some organisms, which are prime suspect of causing prostate infection or prostatitis. One is bacteria Escherichia coli (E coli). Other one can be parasites, like genital viruses, fungi and staphylococci.
Symptoms of Prostate Infection
Infection of prostate can be acute or chronic. In chronic cases infection is recurrent, but less intense than in acute one. Most symptoms are related with urinating, starting from dribbling in the end of it, all trough inability to empty the bladder altogether, and frequent night urinating. In case of prostatitis, high fever and fatigue.Difference between acute and chronic infection is, that in chronic case you can also experience sexual dysfunction, pain in testicles, lower back, urinary pain while urinating, pain in jolts and mild fever.
Tests and Exams
Usually, exam with your doctor starts with digital rectal exam, in order to check the prostate gland. If it is enlarged, doctor may perform other various tests, which include urine tests, bladder, blood, infections, etc. e Doctors exam usually finds, in cases of infected prostate problems like tender testes (epididymitis), and urinary discharge.
Based on the severity of your symptoms, various treatments can be recommended, from lifestyle changes, medications, and in some cases, even surgery.
Treatment and Procedures
In case of acute bacterial prostatitis, it may include:-antibiotics (norfloxacin, Septra, Bactrim etc.) for periods of four to six weeks-in some serious cases of sever bacterial infection or high fever, you may even be hospitalized-in the hospital, you may need installment of catheter (small tube that is inserted in your urethra), in cases of severe infections and obstructions-also in the hospital, the can also give you aminoglycoside or cephalosporins antibiotics
In case of chronic bacterial infection of prostate, effectiveness of antibiotics are limited, because they can not penetrate in to prostate when it is not inflamed. Some other treatments may include:-prostate massage can be introduced, if enlarged prostate blocks the ducts, allowing then to drain properly and enable penetration of antibiotics-your doctor me prescribe to you Bactrim DS and Septra DS type of antibiotics, or some others like Noroxin or Cipro, to boost effectiveness-in cases of relapse of infection after you stopped to take medication, you may need to take them again for 2-3 more weeks, together with prostatic massage
- Prostatitis may be the most prevalent urinary tract disease in patients below 50 years old. According to the statistics, nearly 16% men reported a history of prostatitis at some point in their lives, and prostatitis makes up nearly 25% of urologist visits globally.
- The global annual cost for primary diagnosis and management is a stupendous sum (over $84 million), excluding medical expenditure and cost of the lost productivity, and appears to increase with time. High cost brings invisible economic pressure to patients and the society.
- The National Institutes of Health (NIH) has divided prostatitis into four categories via clinical characteristics, including acute bacterial prostatitis (ABP) (category I), chronic bacterial prostatitis (CBP) (category II), chronic prostatitis/chronic pelvic pain syndrome (CPPS) (category III), and asymptomatic inflammatory prostatitis (category IV).
- The most common among prostatitis is category III, which affects nearly 90% of patients diagnosed with prostatitis. Although the prevalence rate of bacterial prostatitis (approximately 20% of all prostatitis cases) is not the highest in the four categories, ABP carries potential risk of critical morbidity from abscess, sepsis, and septic shock, if insufficiently managed.
- Considering that the evolving changes in resistance rates for fluoroquinolones have a serious impact on treatment, alternative antibiotic therapies are urgently needed. Studies have demonstrated fosfomycin has a strong killing effect in vitro against antimicrobial-resistant E. coli (including ESBL-producing, AmpC-producing, and MDR isolates).
- Phages, bacterial viruses, were used in the treatment of bacterial infections because they show characteristics of infecting and lysing bacteria that have been discovered almost a century ago. Although they were abandoned by the western world after the discovery of antibiotics, the phenomenon of the global effective decline in antibiotic therapy has forced scientists to look for alternative strategies for prophylaxis and control of bacterial infection. Phage therapy may be one of the most popular choices nowadays.
- Antibiotics (levofloxacin and other fluoroquinolones) have been recommended to be the preferred treatment for bacterial prostatitis for years. However, the eradication rates of E. faecalis and E. coli treated with fluoroquinolones vary greatly, ranging between 50%–70% and 70%–90%, respectively. Therefore, much interest has surrounded non-antimicrobial-based approaches. Plant extracts that have long been used for prevention and treatment of urinary tract disorders in traditional medicine are becoming increasingly popular with scholars, especially in this era of antibiotics resistance.
- A multimodal approach to the prolonged antibiotic therapy may be helpful for a higher success rate of bacterial prostatitis. Some studies have reported various effective combination therapies for bacterial prostatitis, including plant extracts and antibiotics.















Your thoughts on this
Loading...