Vagotomy
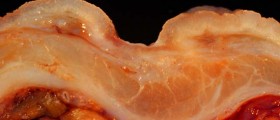
Vagotomy is a surgical procedure in which specific branches of the vagus nerve are resected. The vagus nerve is, among numerous functions, in charge with production of stomach acid. This surgical procedure is performed in patients who do not respond to conventional treatment of peptic ulcers. Namely, all those who suffer from peptic ulcers and cannot control the disease with dietary regimes or all available medications are suitable candidates for vagotomy.
Vagotomy will definitely reduce the production of stomach acid hence reduce or totally eliminate recurrence of peptic ulcers. The surgery can be performed alone or in combination with some other surgical procedure which needs to be conducted due to certain complications of the primary disease.
Types of Vagotomy
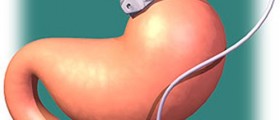
There are more than few types of vagotomy. The very type is determined by the branches of the nerve that are cut. Truncal vagotomy cuts the branches which innervate the stomach, upper organs of the abdomen and upper part of the intestine. This type of vagotomy is performed in patients who suffer from recurrent peptic ulcers and who have already undergone gastric surgery. Selective gastric vagotomy is the procedure in which only nerves that innervate the stomach are severed.
The problem connected to vagotomy is that it considerably affects stomach motility and because of that further surgical procedures such as pyloroplasty or gastroenterostomy are required. They will provide the desirable passage of the food. Another type of vagotomy is selective proximal vagotomy. It deals only with nerves that are in charge with acid-producing segment of the stomach. This way the passage of the food is not disrupted and the there is no need for accompanying surgical procedures.
Complications of Vagotomy
General complications of vagotomy include hemorrhage, infections and unintentional perforation of the stomach. Approximately 20% of all the operated patients complain about problems with stomach emptying. This has been reported in case of truncal vagotomy. These patients need to be further operated and the problem with food passage will be solved.
Diarrhea is not so common complication.
It has been reported in only 1% of all the patients who have undergone proximal gastric vagotomy. The same complication affects only 3% of patients in case that selective vagotomy is performed.
Some patients who have been operated laparoscopically may complain about problems with swallowing.
Similarly to any other abdominal surgery, even vagotomy can be followed by formation of adhesions in the abdomen which may eventually lead to intestinal obstruction.
And finally, in sensitive patients there is chance of reactions to anesthetics.
- The major immediate and intraoperative complications specific to truncal vagotomy include death, bleeding, and injury to the stomach or esophagus. Other complications such as staple line leak, anastomotic leak, and internal hernia may be inherent to the specific type of intestinal reconstruction done.
- The postoperative complications of truncal vagotomy are well documented. Resection of the vagal nerve trunks above the celiac and hepatic branches (differentiates TV versus SV) leads to parasympathetic denervation of the pylorus, liver, biliary tree, pancreas, and small and large intestines.
- Delayed gastric emptying: The stomach loses the vagally mediated receptive relaxation. This leads to an increased intragastric pressure causing an increased emptying of liquids. The pylorus does not relax effectively, and a decrease in solid food emptying is seen. This is the reason the majority of surgeons perform a concomitant drainage procedure at the time of TV.
- Postvagotomy diarrhea: Results from unconjugated bile salts entering the colon, thus leading to osmotic diarrhea. This complication is rarely seen with HSV but is the most common undesirable sequela of TV. It is first treated with codeine/loperamide along with cholestyramine. If this fails, one can consider a reversed jejunal interposition graft.
- Postvagotomy hypergastrinemia: The parietal cells are denervated, causing a decrease in stomach acid output. This leads to G-cell hyperplasia and hypergastrinemia due to the loss of negative feedback mechanisms.
- Ulcer recurrence: TV has the lowest rate of ulcer recurrence compared to the other vagotomies. Recurrence is further prevented with the addition of an antrectomy.
- Dumping syndrome: This typically is seen only when an antrectomy or drainage procedure is done concomitantly with a TV.














Your thoughts on this
Loading...