Tympanoplasty - Overview
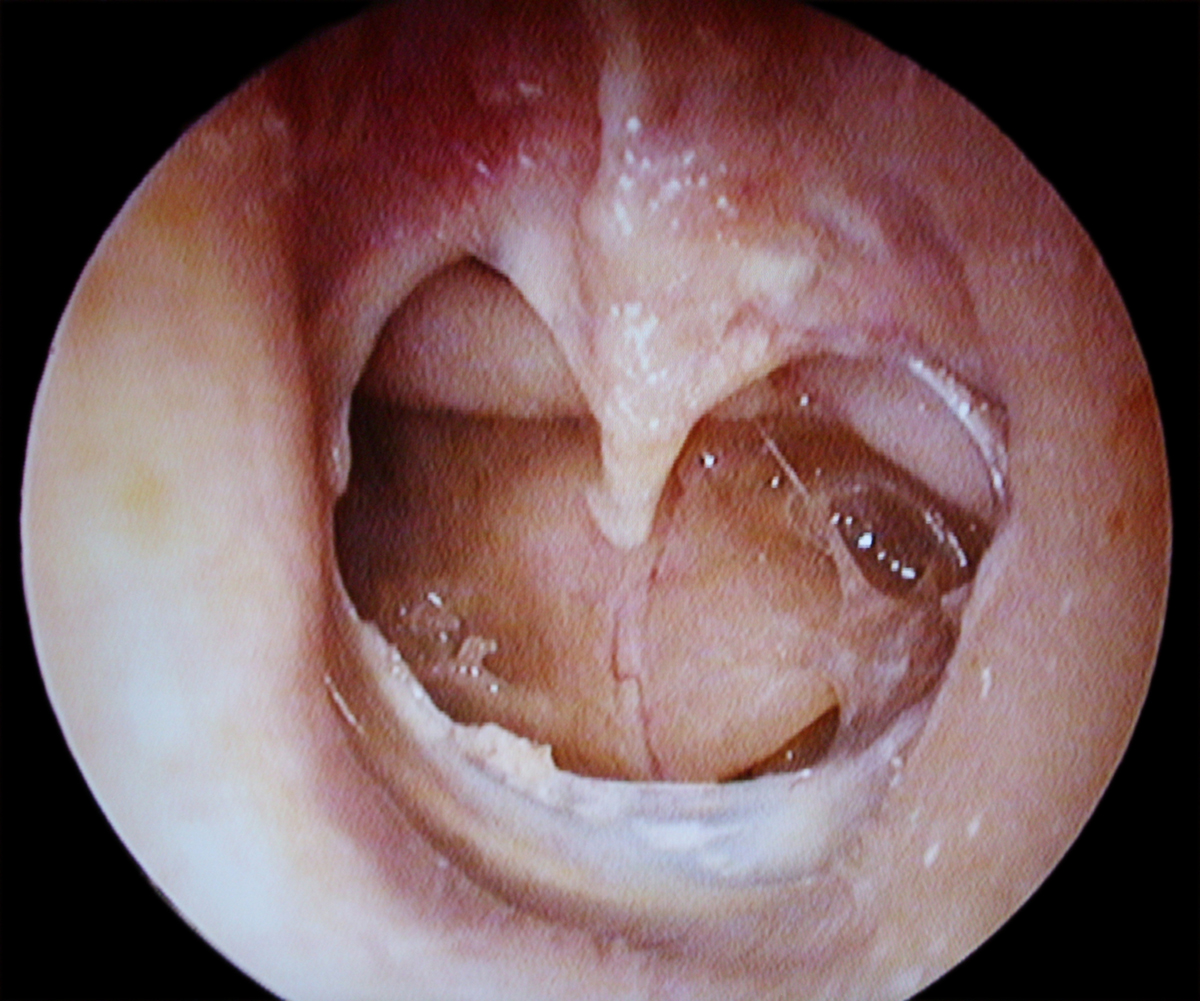
The tympanic membrane is a three-layer structure which separates the outer ear from the middle ear. The rupture is most commonly caused by certain defects in the middle layer which is made of elastic collagen fibers.
Tympanoplasty is a procedure which includes repair of the ruptured ear drum. This is a reconstructive procedure and its goal is to restore the lost function of the ear drum. The perforation may be caused by certain infections such as chronic middle ear infection or be a consequence of trauma to the ear drum. Small perforations do not require surgical repair and they heal spontaneously. On the other hand, if the tympanic membrane is deprived from proper blood supply it simply cannot heal on its own and requires additional help in a form of surgical intervention. In some cases the rupture requires grafting.
Grafts are taken from a vein or fascia of the lobe of the ear. Another option is grafting with synthetic materials usually performed in patients who have already undergone tympanoplasty and have limited graft availability.
Tympanoplasty - The Procedure
There are 5 types of tympanoplasty. Type I also known as myringoplasty is a repair with the assistance of grafts. Type II is performed in case there is also erosion of the malleus. In type III the surgeon reconstructs the tympanic membrane and two ossicles of the middle ear. And finally, type IV and V are performed in more serious damage to the stapes, one of the ossicles of the middle ear.
The procedure may be performed under general or local anesthesia. Patients are discharged after two to three hours after the procedure. They are prescribed antibiotics and pain killers. The patients must keep the operated ear dry and they are not supposed to blow their noses. Majority of patients return to work within six days. Heavy physical labor is banned for several weeks until the wound heals completely.
Surgical repair (tympanoplasty) of the perforated tympanic membrane (TM) is indicated to restore hearing ability as well as to prevent recurrent otorrhea. Tympanoplasty was introduced by Berthold and later developed and modified by Wullstein and Zollner. The various surgical approaches to tympanoplasty include endomeatal (per meatal), endaural, and post-auricular routes. These approaches have a different effect on surgical outcome, depending on the size and site of perforation. A surgical technique using either underlay or overlay of grafts over the perforated TM has been employed by various surgeons. The underlay is widely used and is relatively simple to perform, as the graft is placed entirely medial to the remaining drum and malleus
- A total of 789 tympanoplasties were reviewed, with a male-to-female ratio of 1:1.
- In total, 91% and 9% of tympanoplasties were performed without and with mastoidectomy, respectively. Complete graft take was observed in 98.6% of cases.
- Approximately 25% of patients had an air-bone gap (ABG) gap ?20dB pre-operatively, increasing to 75.6% post-operatively. ABG closure improved from 0.8% to 46.7%. Mean ABG improved from 26.30 ±8.1dB pre-operatively to 14 ± 10.41dB post- operatively. Generally, over 86% of patients had improvement in their hearing function post-operatively.
Risk and Complications of Tympanoplasty
Even though this procedure is highly successful there are several potential complications which may occur. After the procedure which includes grafting there is a slight chance of graft heal failure. This leads to recurrent eardrum perforation. Furthermore, there is also chance of narrowing of the ear canal and scarring and adhesions in the middle ear. Rare complication is a perilymph fistula.
Apart from the previously mentioned some patients may develop facial nerve paralysis, hearing loss, ringing in the ears (tinnitus), and recurrent eardrum perforation and there is also a chance of allergic reactions to drugs. Bleeding and infections are also possible but, even if they occur they are treated successfully.














Your thoughts on this
Loading...