When an examination of the liver has to be performed, a procedure called liver biopsy is done. During this procedure, a part of the liver tissue has to be taken and examined, to make a proper diagnosis of the liver problem. Many different types of liver biopsy can be performed, and all of them will be discussed in this text.
Types of Liver Biopsy
Percutaneous Image-Guided liver biopsy uses a local anesthesia and then an incision is made on the numbed skin. Next, a needle is inserted and guided with ultrasound images or CT, and when the liver is reached, tissue is taken. If needed, this procedure can be performed many times, as much as needed.
Next possible procedure is called percutaneous. This is a very similar procedure, but in this operation, there is no ultrasound or CT use.
The third option is laparoscopic liver biopsy, which can be performed as a part of other operations, or for tissue extraction. The abdomen is the area where the incision is made. Through this incision, instruments are inserted to get the tissue. The most important instrument used is called laparoscope. It significantly decreases the difficulty of performing this operation, since it helps the doctor to see the condition of the liver. Ultrasound can be also used.
Last operation that can be performed is an open surgical liver biopsy. This operation is usually a part of some other procedure. It is rarely done on its own. When this operation is performed, tissue is taken by the wedge or biopsy needle.
These operations are performed for two reasons, either to monitor the progress of treatment or to diagnose the state of the liver. Liver biopsy is a very important procedure, because of them.
Complications
In the first three months following the surgery, hepatic malignancy and advanced liver failure can provoke death, but this is extremely rare. Intraperitoneal hemorrhage is the most common culprit of death after the liver biopsy. Several other complications may arise after the surgery and those are puncture of the lung, viscera, kidney, gallbladder, colon, and pleural effusion.
Also, some problems may be experienced after the surgery. Those problems include hypotension, subclinical bleeding, pain, sepsis, anesthetic reaction, needle problems, and hemobilia.
Intrahepatic arteriovenous fistula is another problem that can be experienced after the liver biopsy. Problems that can happen after the transjugular liver biopsy are cardiac arrhythmias, neck artery puncture, infections, transient dysphonia or Horner's syndrome, liver capsule perforation, and pneumothorax.
- Liver biopsy is invasive and is associated with potential clinical complications. These influence payer and healthcare costs so accurate estimates of complications are required to inform clinical guidelines. Clear contemporary incidences of such complications are lacking, however.
- Even now the quoted incidence of biopsy-related death, 0.01%, is based on a multi-center retrospective report in Italy from over 30 years ago. Similarly, reported incidence of major bleeding varies widely, from 0% to 5.3%, while pain incidence has been rarely reported on, but can reach 84%. Very recently a scoping review on percutaneous biopsy has highlighted age, inpatient status, and coagulation profile as potential factors contributing to bleeding complications, which were estimated to be?2%.
- We systematically searched PubMed and the Cochrane Library for cohort studies reporting on complications resulting from liver biopsy published between 2010 and 2020. Studies on participants of any age and sex, who underwent any percutaneous biopsy for non-focal liver disease, were selected. All events except mild pain, minor hematoma, vasovagal episodes, fever and fistula were defined as major complications. Random-effect model meta-analyses with and without covariates were performed, to examine the effect of publication year, patient characteristics, outcome collection, and biopsy type on incidences.
- We identified 30 studies reporting on complications resulting from percutaneous liver biopsy procedures (n?=?64,356). Incidence of major complications was 2.44% (95% CI 0.85, 6.75), with mortality at 0.01% (95% CI 0.00, 0.11), hospitalization at 0.65% (95% CI 0.38, 1.11), major bleeding at 0.48% (95% CI 0.22, 1.06), and moderate/severe pain at 0.34% (95% CI 0.08, 1.37). Minor complications at 9.53% (95% CI 3.68, 22.5) were mainly pain at 12.9% (95% CI 5.34, 27.9). Technical failure was high at 0.91% (95% CI 0.27, 3.00). Decreasing patient age significantly increased incidence of hospitalization and major bleeding (P?0.0001). Hospitalization incidence also significantly increased with disease severity.
- medlineplus.gov/ency/article/003895.htm
- www.nhs.uk/conditions/biopsy/
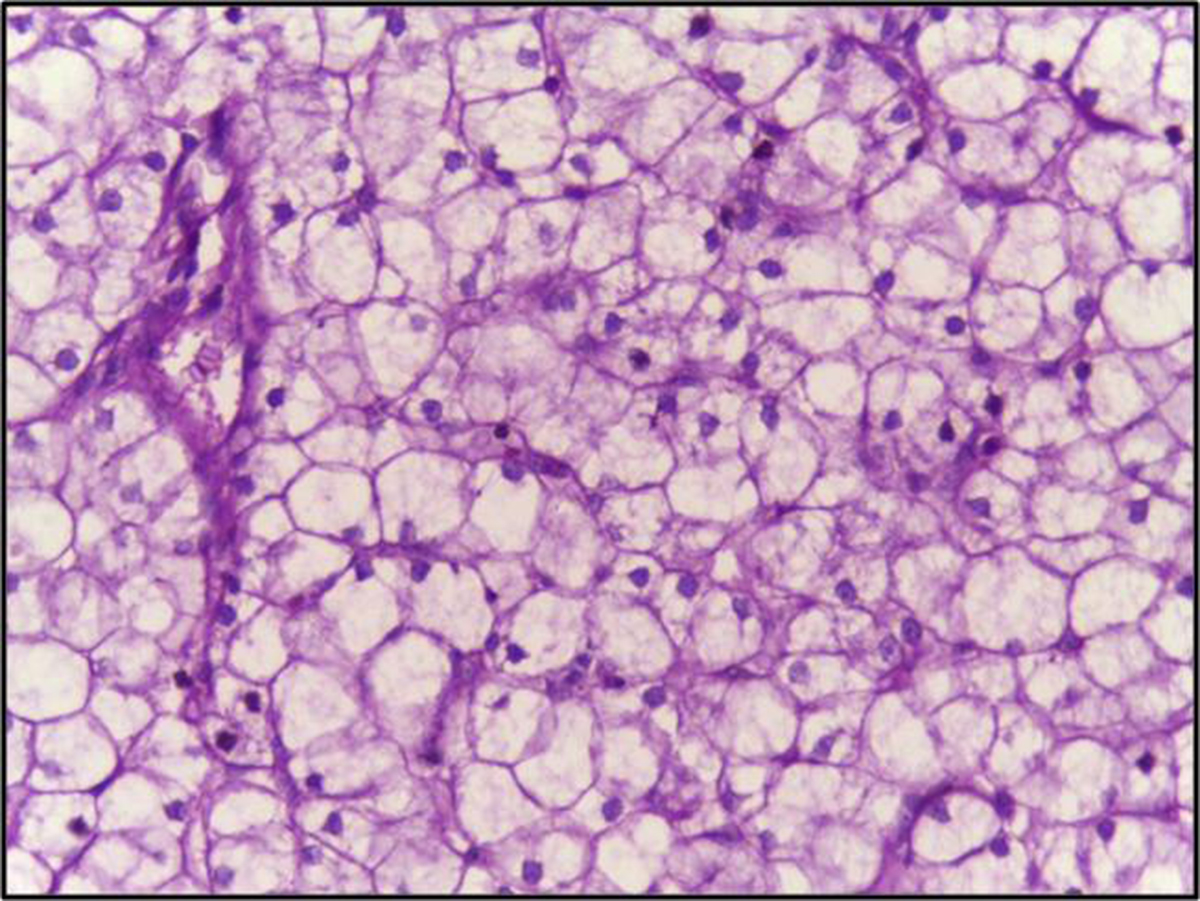
- Photo courtesy of Department of Pathology, Calicut Medical College by Wikimedia Commons: commons.wikimedia.org/wiki/File:Liver_biopsy_of_glycogen_storage_disorder,_PAS_after_Diastase_treatment.jpg
















Your thoughts on this
Loading...