PEG (percutaneous endoscopic gastrostomy) is a surgical procedure that involves insertion of a feeding tube into the stomach through the front abdominal wall. In order for the tube to be placed inside the stomach the surgeon needs to make an incision in the front wall of the abdomen and separate abdominal muscles, enter the peritoneum and finally reach the stomach. This is perfectly achieved with laparotomy so there is no need for open surgery. PEG is generally indicated in patients who have not been or will not be able to take food by mouth for a long period of time.
The technique of placing a feeding tube directly into the stomach was first introduced by Gauderer in 1980. After that several modifications of the procedure have occurred so today surgeons may opt for the most convenient one in the particular case. Nowadays PEG is considered one of the most commonly indicated endoscopic procedures. In the United States between 10,000 and 125,000 individuals undergo this type of surgery annually.
Feeding Tube Placement
The goal of percutaneous endoscopic gastrostomy is to allow patients to introduce food and fluids into their body directly through the stomach. It is highly effective and rather necessary for all the individuals who cannot swallow food/fluids due to certain medical conditions or injuries to the oral cavity and the upper portion of the gastrointestinal tract i.e. esophagus. So, we can say that PEG is also life-saving procedure. PEG is usually performed in a hospital environment, in an operating room. It can be also done in an outpatient surgical facility.
The two major indications for PEG are achieving enteral access for food introduction and gut decompression. For example, people who are suffering from certain neurological disorders may not swallow food properly. This is commonly seen in patients who have had a stroke, those with cerebral palsy, amyotrophic lateral sclerosis etc. Swallowing difficulties also affect individuals in whom there is damage to the upper respiratory or gastrointestinal tract caused by trauma, cancers of different origin or recent surgery. Finally, gut decompression is of major importance for patients with abdominal malignancies that precipitate bowel obstruction or ileus.
Unfortunately, some patients simply cannot undergo PEG. Contraindications for the procedure are classified into absolute and relative contraindication. As for absolute contraindication these include uncorrected problems with coagulation, abnormally low number of platelets, severe ascites, sepsis and intra-abdominal perforation. Furthermore, hemodynamically unstable patients, those with acute peritonitis, abdominal wall infection, history of total gastrectomy are also not suitable candidates and never undergo the procedure. When it comes to relative contraindications these refer to the presence of oropharyngeal/esophageal malignancy, enlargement of the liver/spleen, portal hypertension and associated esophageal varices, ventral hernia, peritoneal dialysis, history of partial gastrectomy or some other abdominal surgeries which may be connected with adhesions or bowel interposition.
How is PEG Performed?
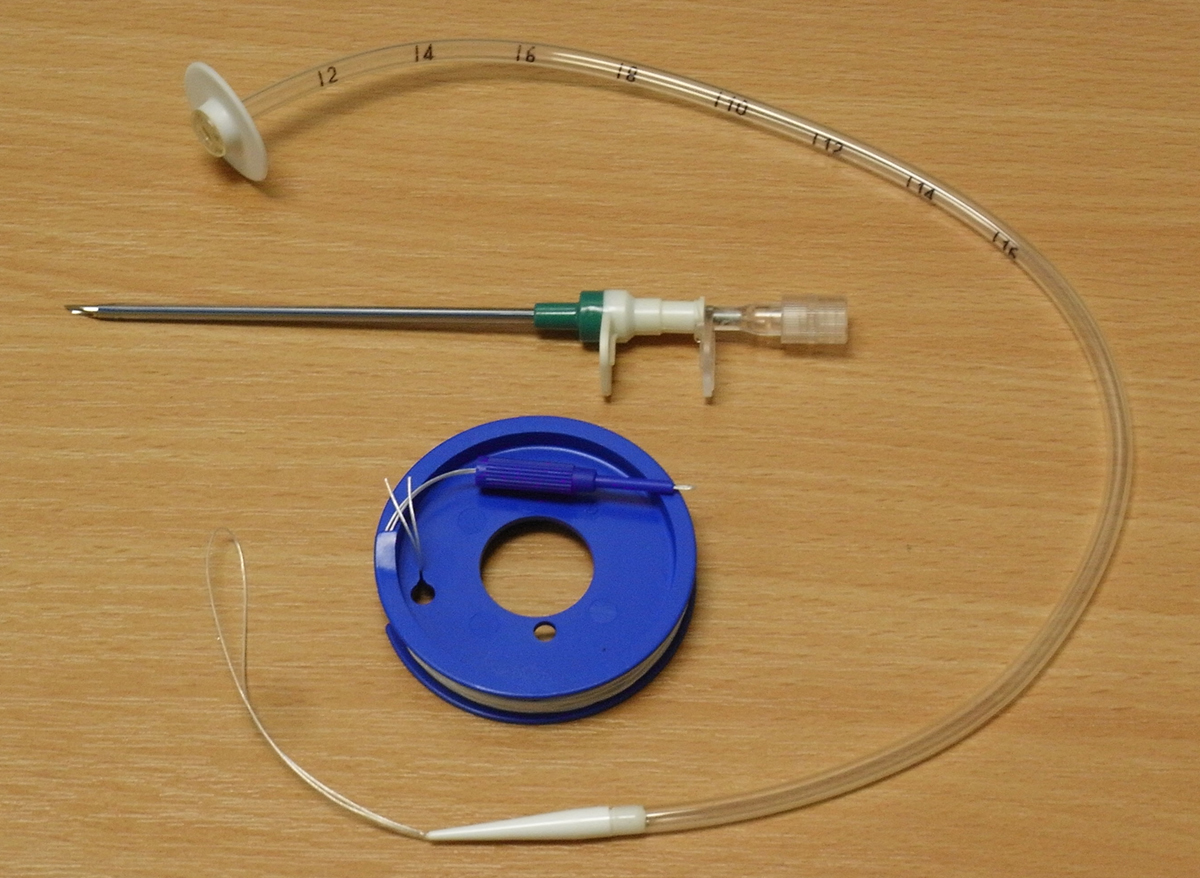
PEG can be performed only by a well-experienced surgeon and if all the instruments and equipment are available. The surgery requires a standard upper endoscope and a PEG kit. Each and every PEG kit contains a PEG tube, guidewire, snare, syringe, needle, sterile fenestrated drape, lidocaine, needle/catheter assembly, surgical blade, gauze, lubricant, scissors and finally swab sticks dipped in povidone-iodine solution.
The first thing a surgeon does is numbing the throat by using local anesthesia (most commonly lidocaine). What follows is placement of an endoscope through the mouth and the esophagus and its final insertion in the stomach. After that the surgeon makes an incision in the front abdominal wall and pushes the needle through the rest of the underlying tissues in order to reach the stomach. After puncturing the front wall of the stomach the tube is inserted and then sutured in place to the skin.
The procedure is relatively simple and not invasive so most patients are actually released the same day the feeding tube is placed. It is,however, possible that the person should stay hospitalized for one more day.
Although it has been routinely performed for many years percutaneous endoscopic gastrostomy may be accompanied by certain complications. The most reported one is definitely infection at the puncture site. The affected skin becomes red, tender and warm. If left untreated, the infection may turn into systemic and trigger sepsis. One more relatively frequent complication is dislodgement of the tube. The tube may also clog. Fortunately, all the mentioned problems are easily dealt with. Most patients successfully avoid infections by receiving antibiotics prophylactically. If the tube moves from its original place, surgeons place it back while clogging can be avoided by following doctor's orders and maintaining impeccable hygiene of the very tube.
Finally, in rather rare cases patients may develop more complex and sometimes even life-threatening complications. Some of these are aspiration, bleeding, pneumoperitoneum, transient gastroparesis or ileus, perforation of the small intestine or the colon, PEG tract tumor seeding, peritonitis and sometimes even allergic reaction to administered anesthetics.















Your thoughts on this
Loading...